In this article, you will learn the types of dry eye disease and its many causes. Our hope is that once you know the types and causes of dry eye disease (DED), we can collectively develop a dry eye treatment plan to help you take control of your DED!
Key Points
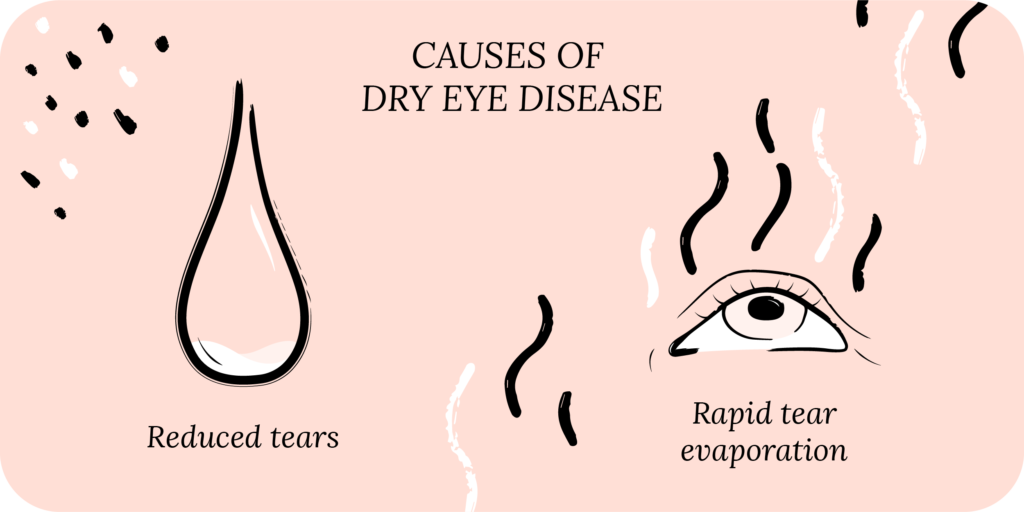
- There are two main types of dry eye disease: aqueous deficient and evaporative. In reality, most forms of dry eye disease are a mix of the two types.
- Aqueous deficient means your body is not making enough tears. Evaporative means your body is making tears, but they evaporate too quickly.
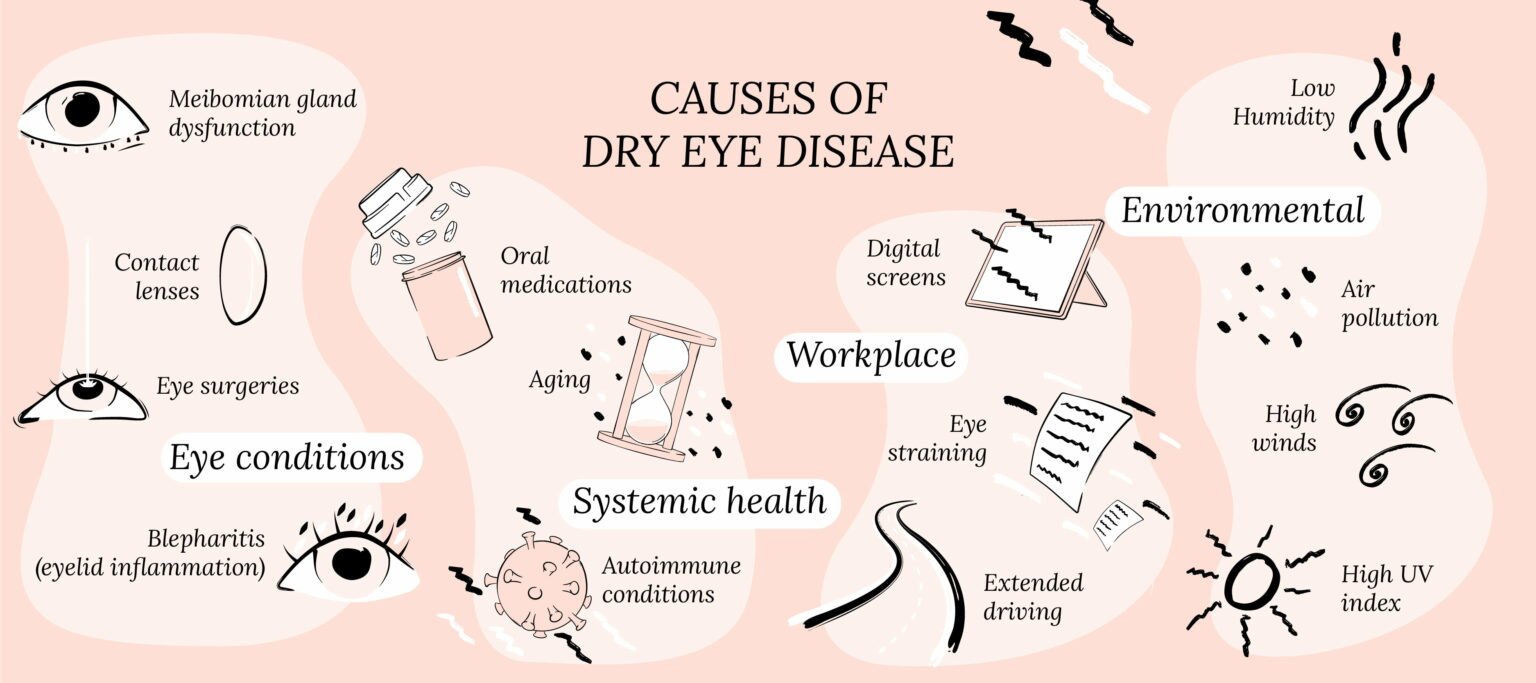
- The environment, work life and numerous eye and medical diseases can all contribute to dry eye disease.
Taking the First Step
First, let us start by saying that dry eye disease (DED) is not your fault. We know it is easy to blame yourself, especially when nothing seems to be helping with your symptoms.
DED is also known as dry eye syndrome, keratoconjunctivitis sicca and ocular surface disease. DED can be divided up into decreased production of tears (aqueous deficient dry eye) or rapid evaporation of tears (evaporative dry eye).1 This is an oversimplification, but it helps with understanding other concepts, such as, how your natural tears are made, the different layers of your tear film, and the basics of dry eye treatment.
Aqueous Deficient Dry Eye: Not Making Enough Tears
Your natural tears come from the lacrimal gland, located in your eye socket deep under the skin. The lacrimal gland produces three different types of tears:2
- Basal tears – always there
- Reflex tears – only when you need them
- Emotional tears – show up due to emotions
Basal tears are constantly secreted to lubricate the ocular surface. Reflex tears are produced in response to stimulation from the cornea. Emotional tears appear during high emotion situations.
Since the lacrimal gland produces your tears, anything that causes it to malfunction will decrease tear production.
Sjögren’s syndrome, an autoimmune condition, causes inflammation of the lacrimal gland, and is associated with severe dry eyes.3 In addition, Sjögren’s affects the salivary glands in your mouth, causing mouth dryness. Patients will complain of “dry mouth” or needing to drink water frequently, in addition to dry eye symptoms.
Exclusive offers
Receive exclusive offers about dry eye health and wellness, courses, and more!
Another cause of decreased tear production is disruption of the connection between the cornea and lacrimal gland. When the cornea is dry, it stimulates the lacrimal gland to produce more tears. This critical link between the cornea and lacrimal gland keeps the ocular surface lubricated, comfortable and protected. If this link is disrupted, tear secretion may decrease. This is often seen in people who have eye injuries, corneal scarring or eye surgeries that decrease the sensitivity of the cornea.
Measuring tear production
Your eye doctor can measure tear production using the Schirmer’s test. This test involves placing a piece of paper on the inside of the lower eyelid and measuring the volume of tears you produce in 5 minutes. If your DED is primarily due to decreased tear production, lubrication with artificial tears can help supplement low tear volume. Your doctor can also place punctal plugs in your tear drainage system to allow your tears to stay longer in your eyes.
Learn more about treatments for dry eyes.
Evaporative Dry Eye: Tears Dry Up Too Fast
In addition to decreased tear production, you could have increased tear evaporation, also known as evaporative dry eye disease. Your tear film is made up of three layers sitting on top of each other:4
- Mucin layer – the glue
- Aqueous layer – the water
- Lipid layer – the oil
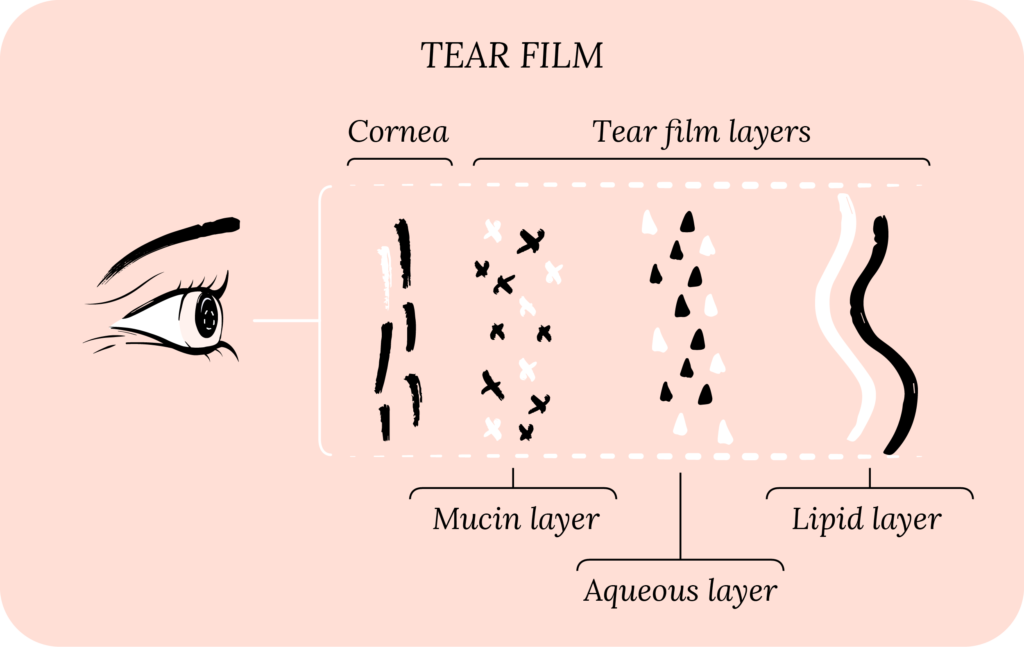
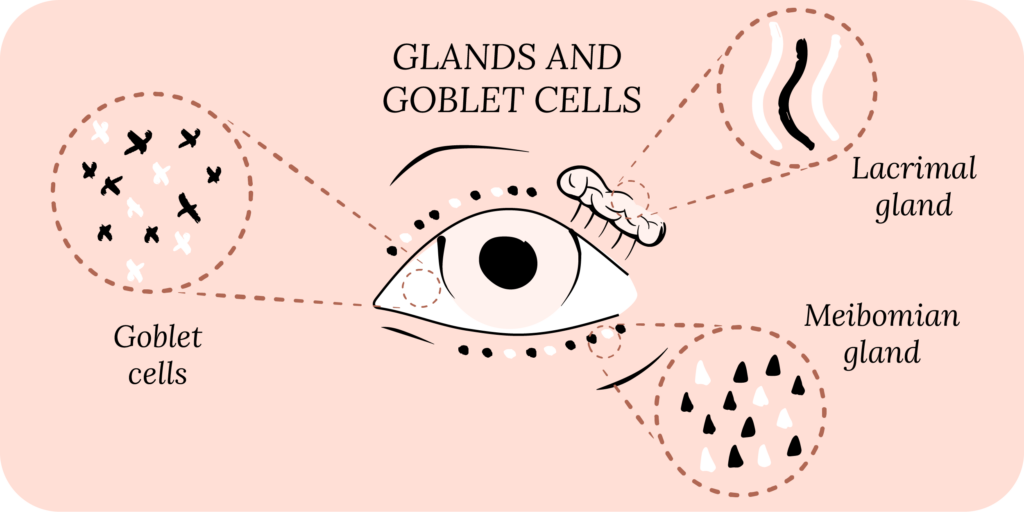
The mucin layer is secreted by cells (especially Goblet cells) located in your conjunctiva. This is the clear film that lines the white part of your eye known as the sclera. The aqueous layer is the largest layer and comes from the lacrimal gland. The lipid layer is made up of oils secreted from your meibomian glands that line the eyelid margin.
The mucin layer is attached to the cornea, the aqueous layer sits on top of the mucin layer, and the lipid layer sits on top of the aqueous layer. All three of these layers work collectively to stabilize the tear film and prevent tear evaporation.

Rest
Warm Compresses
Perfect for eye dryness, fatigue, tearing, and puffiness of the eyelids. Free shipping 📦.
Try today - $30
Meibomian gland dysfunction
The most common cause of evaporative DED is meibomian gland dysfunction (MGD). Meibomian glands line your eyelids and secrete oil which makes up the lipid layer in your tear film. These glands sometimes stop working well. Instead of releasing oil into your tear film, the oil can deposit on the eyelids or in the glands themselves. MGD can happen for many reasons, but it’s mostly related to genetics, environment, age and gender.
When the meibomian glands stop secreting oil, your lipid layer in the tear film becomes deficient. This causes the remaining layers in your tear film to break up and evaporate quickly. Moreover, as the oil builds up on your eyelids or in the meibomian glands, you can get styes and eyelid inflammation, also known as blepharitis. This creates a vicious cycle where MGD directly causes DED, leading to other conditions that worsen dry eye disease.
As we discussed above, if the lacrimal gland malfunctions, you can get decreased tear production. Meaning, your aqueous layer may become deficient, which leads to overall tear film instability and rapid tear evaporation.
Eye injuries
If your conjunctiva gets injured or damaged, the cells in it may not produce the molecules necessary for the mucin layer. Without mucin, the remaining layers of the tear film lose their anchor and become unstable. We can see this in eye injuries, such as blunt trauma and chemical exposure (acids and alkali), where the conjunctiva can get scarred.
If the surface of the cornea is damaged, the mucin layer may not be able to attach to it. This can happen in the setting of eye injuries, corneal scarring, and eye surgeries. If the mucin layer fails to attach to the surface of the cornea, the aqueous and lipid layers also will not attach well, and as a result, the tear film can become unstable and evaporate quickly.
We can measure tear film instability in the clinic by using fluorescein, which is the “yellow” stuff that eye specialists put in your eyes. Fluorescein is a natural dye, and it lights up when we use a special light on our exam machine. With this, we can see how quickly your tear film breaks up (TBUT). A rapid TBUT is an indicator of tear film instability.
When we see this, we may think about using artificial tears with oil and lipids. We also emphasize eyelid hygiene with warm compresses, cold compresses and eyelid wipes to improve meibomian gland function.
You can learn more about treatments for dry eyes here.

Foundation
Eyelid Hygiene Plan 2
Perfect for eye dryness, burning, itching, crusting/flaking of eyelashes and inflamed eyelids. Free shipping 📦.
Try today - $45
Mixed Forms of Dry Eye Disease
Most patients do not have a clear aqueous deficient or evaporative type of DED. For example, as we discussed above, decreased tear production from the lacrimal gland can lead to both types of DED. Eye injuries, scars and surgeries can also lead to both. In fact, the most common types of dry eye disease are typically a mix of aqueous deficient and evaporative. Further, there are several contributing factors, such as the environment, workplace, ocular diseases, medical problems and oral medications.
Environmental Causes of Dry Eye
Your environment plays a vital role in DED.5 For example, high winds or low humidity may cause your tears to evaporate fast. Poor air quality may cause irritation to your eyes. A high ultraviolet (UV) index (intense sunlight) could be difficult for people who experience light sensitivity because of DED.
These factors are also important to consider inside your house. Sleeping under a fan or in front of an air conditioner could cause your tears to evaporate rapidly, just like in high wind areas. Other risk factors include low humidity inside your house and stagnant, poor air quality.
With COVID-19, wearing masks has become standard practice. For DED patients, this becomes a problem because airflow is directed upwards toward your eyes, leading to rapid tear evaporation. This causes dry eyes and actually carries the name “mask-associated dry eye disease.”
You should certainly wear a mask during the pandemic, and if you have DED and live in areas with environmental risk factors, you do not need to pack your bags and move. Your environment should not be your enemy! Instead, you can make small, but impactful changes to improve your dry eye symptoms. For example, using a humidifier, and directing air conditioning away from your eyes can make a big difference. So can wearing sunglasses or eye protection when outside on sunny or windy days.
Occupational Causes of Dry Eye
The average person spends at least half of their waking hours at their job. For most of us, that means looking at a computer screen for hours. When we look at a computer screen, or any screen for that matter, our blinking decreases, and so we do not replenish our tear film, leading to dry eye symptoms.6
Another important consideration is screen placement. If your computer screen is above eye level, your eyes naturally open more to look upwards at the screen. This exposes more of your ocular surface to the environment.
With COVID-19, we have become even more reliant on our computers for work. Anytime we are using our eyes to focus, our blinking naturally decreases. This includes driving, cooking, knitting, sewing, you name it.
Most of our daily activities require focusing with our eyes, which is why dry eye disease can be so debilitating.

Rescue
Cold Compresses
Perfect for sudden flare-ups of eye dryness, pain, burning, and swollen/inflamed eyelids. Free shipping 📦.
Try today - $12
Other Eye Conditions Linked to Dry Eye Disease
There are several eye conditions and surgeries that can cause or worsen DED.7 For instance, the drops used to lower your eye pressure in glaucoma cause dry eyes.
Antibiotics used to treat corneal or eye infections can lead to DED if used for too long. Most of these eye drops contain benzalkonium chloride (BAK), a preservative that prolongs the shelf-life of eye drops. This can be toxic to the ocular surface, including both the cornea and conjunctiva.
Contact lens wear is another cause of dry eyes. Millions of people worldwide wear contact lenses. Many do not follow good contact lens hygiene, such as not sleeping or showering in contact lenses, or discarding them at the recommended time. Poor contact lens hygiene can directly injure the cornea, leading to DED. Contact lenses may also destabilize your tear film and blunt the connection between the cornea and the lacrimal gland. This leads to decreased tear production.
Eye surgeries can also cause or worsen different types of dry eye disease. Eye surgery can directly injure the ocular surface, and typically involves antiseptics and drops that are not gentle on the cornea.
Refractive surgery, such as LASIK, can injure the corneal nerves and the Goblet cells (which secrete mucin for your tear film), and change the shape of the cornea, leading to tear film instability and decreased tear production.
Medical Problems Linked to Dry Eye Disease
Did you know that your general health can also impact DED?8
Autoimmune conditions, such as Sjögren’s syndrome or rheumatoid arthritis, are associated with types of dry eyes. Thyroid problems can manifest with thyroid eye disease, which typically causes dry eyes.
Poor nutritional status (diet with low vitamins A, B, C, D and E, and low omega-3 fatty acids) can contribute to dry eye disease. Cancer, dermatitis, rosacea, diabetes, high blood pressure, and menopause (hormonal changes) are a few of the many medical problems associated with dry eyes.
Several oral medications have side effects that can cause dry eye symptoms. These medications include antihistamines, antidepressants, birth control pills, isotretinoin (Accutane), diuretics, decongestants, beta blockers, chemotherapy, and hormone replacement therapy. These medications can either decrease tear production or make your tear film unstable.
Putting It All Together
As we’ve said before, and the above article should convince you, DED is not just about dry eyes; it can affect and be affected by your whole body and mind leading to poor quality of life.
DED is not your fault!
While it is important to know the causes and types of dry eyes, remember that most forms of DED are usually multifactorial, with several contributing factors. This is why simple eye lubrication with eye drops or CorneaCare artificial tears, warm compresses and even prescriptions (cyclosporines and lifitegrast) alone are insufficient.
What is most important is to develop a personalized therapeutic plan, make some important environmental and lifestyle modifications, and stay consistent.
What’s Next
Let’s learn about why dry eye disease matters! Also read more to learn about the causes dry eye disease.