What Artificial Tears Do for Dry Eyes
The typical dry eye patient spends months trying to manage their symptoms before seeing an eye doctor (ophthalmologist or optometrist). This usually means a trial-and-error approach with various over-the-counter (OTC) eye drops, eyelid wipes, compresses, gels, ointments and oral supplements. This leaves most patients feeling frustrated and helpless, and without relief from dry eye symptoms. While OTC treatments can certainly help, they need to be done consistently and be tailored to your specific needs, overall eye health, and lifestyle.
Eye lubrication is an essential part of dry eye treatment. While eyelid hygiene works to stabilize your tear film, lubricating eye drops, gels and ointments replenish your tear film, providing relief.
Key Points
- A patient with dry eyes can spend months even years experiencing symptoms before seeing an eye doctor.
- Eyelid hygiene stabilizes your tear film, while lubricating artificial tears replenish your tear film.
- The “best dry eye drop” is the one you use consistently as instructed.
What is Dry Eye Disease
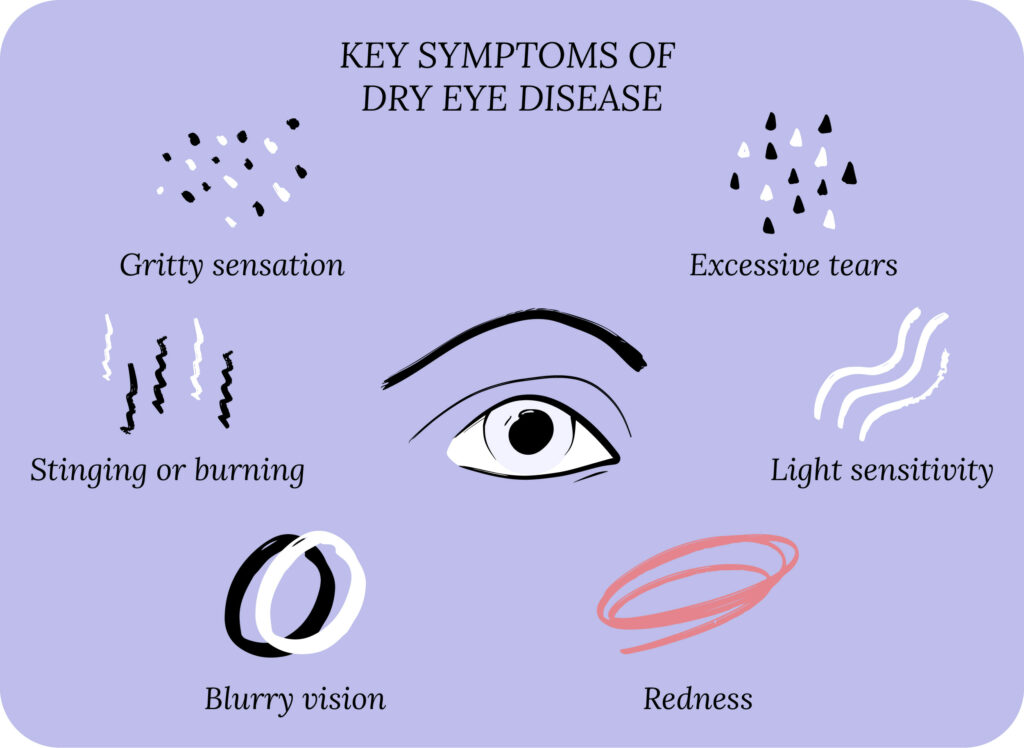
Let’s first review some basics before we dive into artificial tears. Dry eye disease (DED) is also known as dry eye syndrome, keratoconjunctivitis sicca and ocular surface disease.1 The classic dry eye symptoms are blurry vision, light sensitivity, itchiness, watery eyes, dryness, stinging or burning, red eyes, gritty sensation, and eye pain.
Dry eyes can be caused by many things, but we can break them down into two categories: aqueous deficient and evaporative. With aqueous deficient DED, your lacrimal glands do not produce enough natural tears to lubricate the surface of the eyes (the cornea and conjunctiva). With evaporative DED, your body’s tear production is normal, but the tears evaporate too quickly. In practice, DED is a combination of both aqueous deficient and evaporative, leading to tear film dysfunction.
The environment and lifestyle play an important role in dry eye disease. Environmental factors, such as low humidity, high winds and air pollution can worsen the symptoms of dry eye. Lifestyle risk factors include extended use of digital screens, wearing contact lenses, poor diet, decreased hydration, and smoking.
Dry eye disease can impact you on many levels, including physically, emotionally, financially and even socially. Starting a treatment plan can lead to dry eye relief, and help prevent any long-term side effects and eye problems.
Our Community
Chat, share, and learn from our doctors, coaches and others like yourself
👩⚕️ Get answers!
How to Treat Dry Eyes
One way to think about dry eye treatment is to link it with the causes of dry eye disease. In aqueous deficient DED, lubricating eye drops can augment the deficient tear production. In evaporative DED, eyelid hygiene can treat meibomian gland dysfunction, which leads to improved lipid secretion and stability of the tear film. A good treatment combines lubrication with reduced tear evaporation, but also addresses environmental factors and lifestyle.2 What is good for your eye care should also be good for your overall health care.
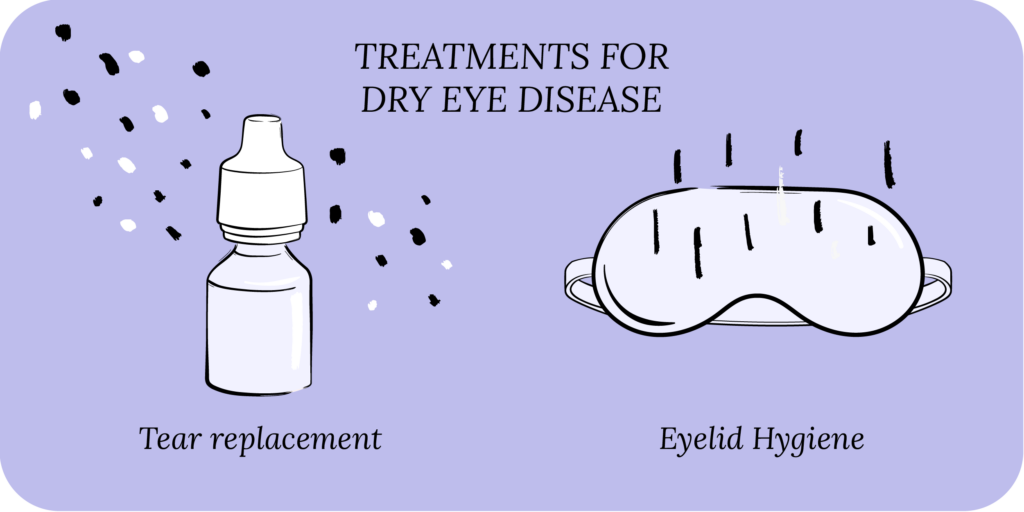
The treatment options for dry eye include OTC lubricant eye drops (artificial tears), eye gels, eye ointments and eyelid hygiene (warm compress and eyelid wipes). Using a humidifier can be helpful, as can taking an oral dry eye supplement. In some cases of severe dry eyes, a person may require prescription eye drops (Restasis, Xiidra and Cequa) and in-office procedures.

Foundation
Eyelid Hygiene Plan 2
Perfect for eye dryness, burning, itching, crusting/flaking of eyelashes and inflamed eyelids. Free shipping 📦.
Try today - $45
Artificial Tear Drops
Dry eye treatment starts with eyelid hygiene and lubricating eye drops. Artificial tears replenish your tear film and supplement your natural tears, protecting your cornea, making your eyes feel comfortable, and keeping your vision clear.

While artificial tears are important, finding the right artificial tear for your eyes can be difficult. There are over 50 different types of artificial tears on the market (think of the eye drop aisle in your local drug store).
While it’s good to have options, many patients feel overwhelmed by the large variety. Moreover, the way companies market the tears can also be confusing. For example, should you use a standard artificial tear, or a rewetting drop if you wear contact lenses? Or a tear marketed to work against digital screens? How about antihistamine drops for allergies? Or pink-eye drops? And the list goes on.
All of this causes patients to try several types of artificial tears without being consistent with one, which is often more important.
Artificial Tear Gel and Ointment
In addition to eye drops, artificial tear gels and ointments can also provide lubrication to the surface of the eye. Typically, gels and ointments will cause blurry vision, so they work best if used right before bedtime to provide lubrication overnight.3 For people waking up with dry eyes, overnight lubrication can make a significant impact. In patients with severe dry eyes, gels and ointments can also be used during the day, as they provide better lubrication than eye drops.

Rise
Eyelid Wipes
Perfect for eye dryness, itching, burning, and crusting/flaking of eyelashes. Free shipping 📦
Try today - $25
Preservatives or No Preservatives?
Artificial tears come in two major classes: those with preservatives, and those without preservatives. The most common preservative is benzalkonium chloride (BAK). While preservatives make the artificial tears last longer on the shelf, they can have adverse effects on the surface of the eye, and can actually worsen DED in the long run.
How often the eye is exposed to preservatives makes a big difference. For example, with eyelid wipes, since you only use them 1-2 times a day and don’t apply them directly to your eyeballs, the impact of preservatives from eyelid wipes may be insignificant. However, preservatives really start to have negative effects if you’re exposed to them more than 3-4 times a day on a long-term basis.4 This is why it’s best to use preservative-free eye drops when possible.
Preservative-free artificial tears typically come in small single-use vials, which need to be handled with care. While these small vials should be discarded after each use to prevent contamination, most people will typically use the same vial multiple times. Recently, two new multi-use bottles have been created that can dispense preservative-free artificial tears without contamination for up to 90 days after opening.
“The Best Eye Drops”
Now we get to the question that every dry eye patient asks: “What is the best eye drop?” Sorry to break it to you, but there is no “one” best eye drop. The honest answer is that the best eye drop is the one you use consistently as instructed. Typically, you want to use artificial tears 4-6 times a day, and if you can do that consistently, you will see relief. But the truth is most patients want immediate relief, and if one drop doesn’t work, they quickly move on to the next. This sets the stage for a trial-and-error process that doesn’t provide relief, is frustrating, and costly. We want you to avoid this!
It is important to use an artificial tear as instructed for at least 1-2 months before deciding it’s “not working.” You may not immediately feel relief, but remember that DED is a chronic condition, so the treatment also takes time to work. And once you do get dry eye relief, don’t stop the artificial tears! You may be able to decrease the number of times you use the tears, but stopping them entirely may cause your symptoms to recur.

Rest
Warm Compresses
Perfect for eye dryness, fatigue, tearing, and puffiness of the eyelids. Free shipping 📦.
Try today - $30
Common Ingredients in Artificial Tears
Artificial tears can have many ingredients which address different aspects of the tear film. Your tear film contains three layers: mucin (sticky stuff), aqueous (water), and lipid (fat). The mucin layer sticks to the cornea, the aqueous layer is the water, and the lipid layer protects the other layers and seals in the lubrication. Artificial tears are designed to supplement the deficient aqueous or lipid layers. We also know that in DED, your tears can be highly concentrated (more salt than water), which can lead to ocular surface injury. Artificial tears can contain osmoprotectants that shield the ocular surface from highly concentrated tears.
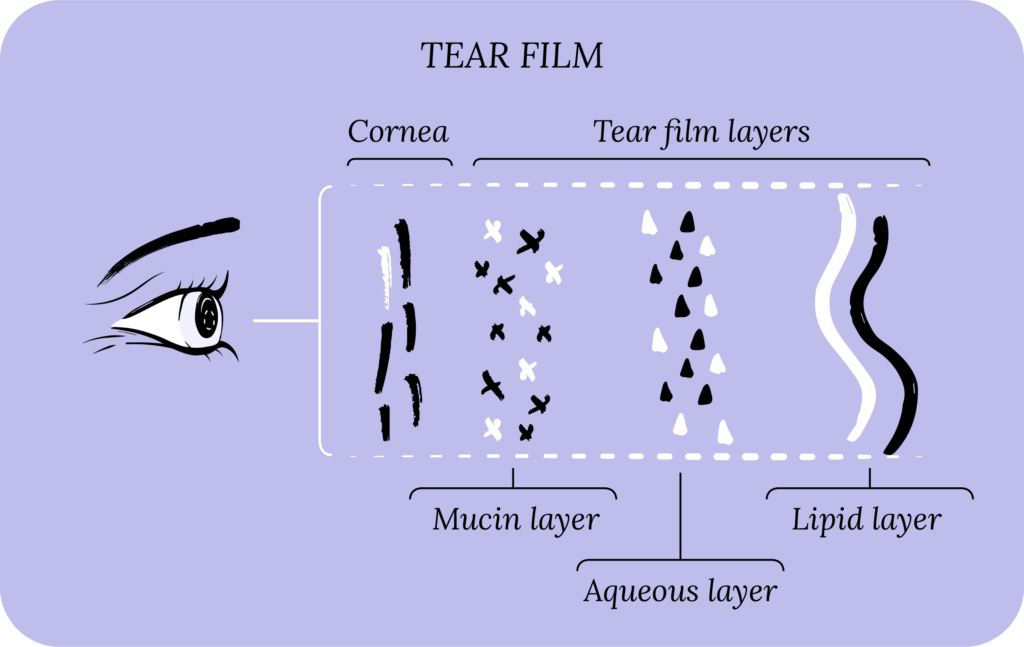
Common artificial tear ingredients can be broken down into four categories. Note that many of the ingredients can perform multiple functions.5
- Demulcents: soothe and protect irritated and inflamed tissue. Many demulcents also serve as emollients, which may soften the ocular surface. Demulcents typically appear as the “active ingredients” on the artificial tear packaging. Examples include: carboxymethyl-cellulose (CMC), hydroxypropyl methylcellulose (hypromellose), hydroxyethylcellulose, methylcellulose, dextran 70, gelatin, glycerin, polyethylene glycol (300,400), polysorbate 80, polyvinyl alcohol, and polyvinyl pyrrolidone (povidone).
- Humectants: hydrate and moisturize by attracting water. Examples include: hypromellose, dextran, propylene glycol, glycerin and hyaluronic acid.
- Occlusives: create a barrier over your skin to prevent the water from evaporating away, and lock in the moisture. Examples include: mineral oil, flaxseed oil, castor oil, paraffin, lanolin, and petrolatum.
- Osmoprotectants: shield the ocular surface from stress-injury caused by highly concentrated tears (more salt than water). Examples include: trehalose, erythritol, and levocarnitine.

All Rounder
Eyelid Hygiene Plan 3
Perfect for eye dryness, burning, itching, grittiness, crusting/flaking of eyelashes and inflamed/swollen eyelids. Free shipping 📦.
Try today - $60
How to Use Eye Drops, Gels and Ointments
Many patients struggle with properly using eye drops, gels and ointments.
The most important thing is to make sure you use these products safely. This all starts with preventing contamination of the bottle tip or tube tip that contains the drops or gel/ointment. For proper use, wash your hands, open the cap, and don’t touch the tip with your hand, or any other surfaces.
For artificial tear drops, tilt your head back, pull your lower eyelid down and place a drop in the eye. Take care not to touch the eyeball with the tip. If you struggle, you can place a drop in your medial canthus instead. The medial canthus is the corner of the eye where the upper and lower eyelids meet by the nose. To do this, tilt your head back, close your eyes and place a drop in the medial canthus. Then open your eyes and let the drop flow in. It’s not perfect, but it helps.
For gels and ointments, pull down your lower eyelid, look up, and place about 1cm of gel or ointment in the inferior fornix. The inferior fornix is the pocket between your lower eyelid and the eyeball. Again, take care not to touch your eyeball with the tip.
At the end, cap the tip and be careful not to touch it. Store as instructed on the packaging.
Putting It All Together
Your eyes and eyelids work in union to protect your eyes and maintain your tear film for comfort and clarity. Eyelid hygiene improves the function of meibomian glands in your eyelids, which helps stabilize your tear film. Lubricating artificial tears augment this by replenishing your tear film. Sometimes eyelid hygiene alone relieves symptoms, but you may need both eyelid hygiene and lubrication for lasting dry eye relief.
What’s Next
We really think everyone should take our Dry Eye 101 course. Find it here!
If you’ve already taken it, amazing! Check out more articles in the Continuing Education section below.




