Key points
- There are several procedures available for dry eye treatment, including punctal plugs, intense pulsed light and Lipiflow.
- Procedures may be a good option for some patients, but they work best when used as a supplement to, and not a replacement for, a good overall treatment plan.
- Most dry eye treatment procedures are not covered by insurance, and can range from $500 – $1500 per treatment.
Keywords
iLux, LipiFlow, intense pulsed light, NuLids, punctal plugs
Taking the first step
We know dry eye treatment can be challenging, especially without the right support and guidance. Eyelid hygiene, eye lubrication, and lifestyle changes can be tough to keep organized and follow consistently, even if they may be working. Dry eye patients may find all this overwhelming and frustrating, and therefore end up turning to “magic cures” or “quick fixes” for dry eyes, including prescription drops and procedures.
Just like with prescription eye drops, procedures for dry eyes can be a good option for some patients. However, you should remember a few key points when considering procedures.
- Most insurance companies do not cover procedures for dry eye treatment, and can range from $500 – $1500 per treatment.
- Not every eye doctor has access to the equipment needed to perform these procedures, so access can be limited.
- Dry eye procedures are often marketed as “quick fixes,” but you’ll often need multiple follow-up treatment sessions to see results and maintain them.
Most importantly, like with prescriptions, procedures work best when used in conjunction with a good overall treatment plan, which includes eyelid hygiene, artificial tears, good nutrition and hydration, and important lifestyle changes. Your eye care and eye health reflect your overall general health, and what’s good for the eyes should also be good for the mind and body.
What is dry eye disease
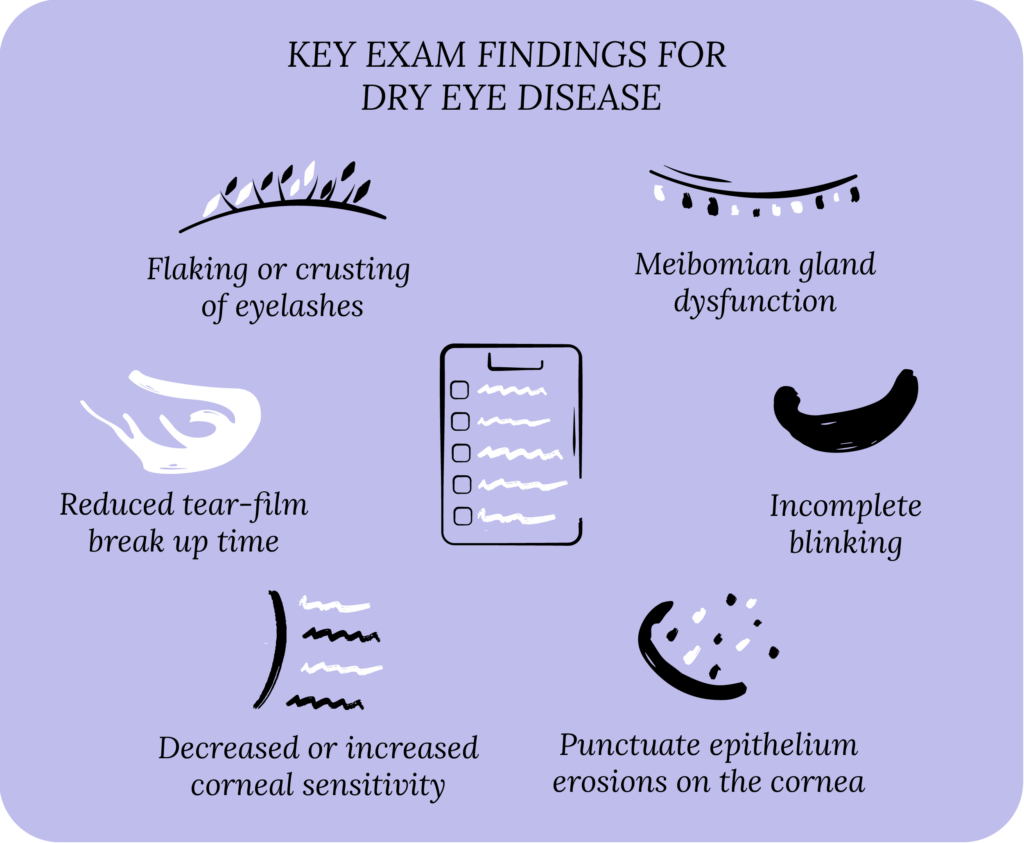
Let’s quickly cover some dry eye basics before diving into procedures.1 Dry eye disease (DED) is also known as dry eye syndrome, keratoconjunctivitis sicca and ocular surface disease. The usual symptoms of dry eyes are blurred vision, gritty sensation, light sensitivity, watery eyes, dryness, burning sensation, and red eyes.
DED can be classified as aqueous deficient and evaporative. With aqueous deficient dry eye, your lacrimal glands don’t produce enough natural tears to lubricate the surface of the eye (the cornea and conjunctiva). With evaporative dry eye, your body makes enough tears, but the tears evaporate too quickly. Evaporative DED is more common than aqueous deficient, but most patients typically have some components of both, causing tear film instability.
Risk factors for dry eyes include pre-existing ocular conditions, such as meibomian gland dysfunction (a problem with oil glands in the eyelids), blepharitis (eyelid inflammation), glaucoma and eye surgery. Medical conditions, such as Sjögren’s syndrome, rheumatoid arthritis, menopause, diabetes and high blood pressure are also risk factors. Oral medications, such as antihistamines, antidepressants, birth control pills, decongestants, and beta blockers can cause and worsen DED.
Lifestyle risk factors for dry eye include extended use of digital screens, poor diet, wearing contact lenses, and smoking. Environmental risk factors include dry climate (low humidity), air pollution, high winds and air allergens.
DED can affect you on my levels, including physical, emotional, financial and even social wellbeing. Starting a treatment plan for dry eyes can help you get relief and prevent long-term complications and eye problems.
Basics of dry eye treatment
Dry eye treatment addresses the two classes of DED. Eye drops (artificial tears), gels, and ointments to supplement your tear film. Eyelid hygiene (warm compresses and eyelid wipes) can stabilize your tear film and prevent tear evaporation. Nutrition and hydration also play a key role, which includes drinking lots of water and eating a well-balanced diet (vitamins, minerals and fatty acids). An oral dry eye supplement can address any deficiencies in your diet. In some cases of severe dry eyes, a patient may require prescription eye drops, oral prescription medications, and procedures for dry eye treatment.

Foundation
Eyelid Hygiene Plan 2
Perfect for eye dryness, burning, itching, crusting/flaking of eyelashes and inflamed eyelids. Free shipping 📦.
Try today - $45
Procedures for dry eye treatment
In the last decade, multiple procedures have become available for dry eye treatment.2 The Food and Drug Administration (FDA) has approved many of these procedures, with several others in the pipeline. These procedures are usually done by eye doctors (ophthalmologists and optometrists) in a clinical setting.
Most dry eye procedures focus on five major categories:
- Tear drainage system
- Meibomian gland dysfunction and eyelid inflammation
- Tear production and lubrication
- Corneal healing
- Eyelid and conjunctival surgery
In the below sections, we’ll go through each category and highlight some of the common procedures available for dry eye treatment.
Procedures for the tear drainage system
The most common procedure performed for DED is punctal plugs, aka lacrimal plugs.3 To understand how punctal plugs work, we must first understand how your natural tears leave your eyes. Your tear drainage system, aka naso-lacrimal drainage system, is composed of four puncta (2 for each eye: 1 in the upper eyelid and 1 in the lower eyelid). These puncta are tiny openings on your eyelid margin near the nasal bridge where the eyelids come together, and are typically referred to as tear ducts. These puncta drain tears into the superior (upper eyelid) and inferior (inferior eyelid) canaliculi, which combine to form the common canaliculus. The common canalicular drains into the lacrimal sac, and then into the back of your nose through the nasolacrimal duct, and eventually to the back of your throat.
Punctal plugs
Punctal plugs block the puncta and prevent tears from draining, which may increase the total volume of tears in your eyes and improve your tear film. Punctal plugs can be made from various materials. Temporary plugs are made from absorbable collagen, and typically last 1-2 weeks before dissolving. These short-term collagen plugs are best used before or after eye surgery (LASIK and cataract surgery) to prevent the onset of dry eyes, or to determine if a DED patient gets relief from temporary punctal occlusion before trying more long-term options.
Semi-permanent and permanent punctal plugs are made from non-dissolvable silicone, and can last six months to several years. These silicone plugs are typically used in patients with DED. Other materials include acrylic, hydrogel and polydioxanone.
Canalicular plugs
While punctum plugs are placed in the puncta, canalicular plugs are placed in the canaliculus farther along the tear drainage system. Canalicular plugs are typically made from the same material as semi-permanent and permanent punctal plugs. Because of their deeper placement, canalicular plugs are thought to be a more permanent, long-term solution compared to punctal plugs.

Rise
Eyelid Wipes
Perfect for eye dryness, itching, burning, and crusting/flaking of eyelashes. Free shipping 📦
Try today - $25
Plug placement and complications
Punctal and canalicular plug placement is done in the clinic. The eye doctor does the following:
- Examine the puncta, to determine the appropriate size of the plug. We typically use the puncta in the inferior eyelid because patients tolerate it better compared to the upper eyelid puncta.
- Place a topical anesthetic at the site of the puncta, such as proparacaine drops or lidocaine gel, although this isn’t often necessary.
- Use a dilator to open up the puncta.
- Insert the plug into the puncta to the desired depth using the inserter. For punctal plug insertion, typically the end of the plug has a cap that rests near the top of the puncta. A canalicular plug is inserted deeper and the end cannot be easily seen after placement.
- Most plugs come preloaded onto an inserter, but others may require loading the plug manually onto the inserter using forceps.
The main complications of punctal and canalicular plugs are extrusion or migration. Extrusion is when the plug is poking out of the puncta, and can either irritate the eyes or fall out. Migration is when the plug moves down the tear drainage system further than intended. Extrusion is mainly a problem with punctal plugs, which is why finding the best fitting plug is key. Migration is mainly a problem with canalicular plugs, and sometimes removing these may require surgery.
Other common side effects include epiphora (excessive tearing) and foreign body sensation near the plug placement. Less common complications include an allergic reaction to plug material, infections around the plug, and plug migration outside the tear drainage system.
Punctal and canalicular plugs are typically avoided in patients who have concurrent blepharitis or other forms of eye and eyelid inflammation. The plugs could serve as a source for ongoing inflammation, and prevent the drainage of inflammatory markers in the tear film, which may actually worsen dry eye symptoms. This underscores the importance of doing a good eye exam before placing plugs.
Punctal cauterization
In patients who cannot tolerate plugs because of the above-listed complications and side effects, a final option is punctal cauterization. During this procedure, the eye doctor uses a heated tip to warm the puncta, which causes it to scar and close permanently. A topical anesthetic is typically applied before this procedure.
Punctal cauterization is typically reserved for patients with severe DED, and those who cannot tolerate standard plugs. The reason is that most patients will get epiphora after cauterization, and their symptoms may worsen if they develop blepharitis in the later stages of their disease progression.
Procedures for meibomian gland dysfunction and eyelid inflammation
The most common causes of DED are meibomian gland dysfunction (MGD) and blepharitis.4 Meibomian glands line the inner eyelids, and secrete lipids (oils) which form the lipid layer of your healthy tear film. This lipid layer prevents tear evaporation and protects the remaining layers of your tear film (aqueous layer from the lacrimal gland and mucin layer from the goblet cells).
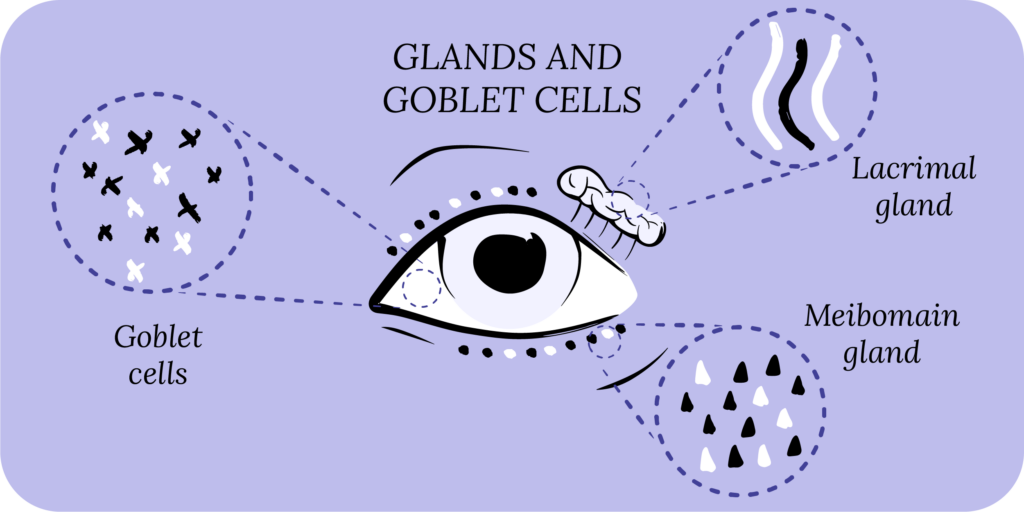
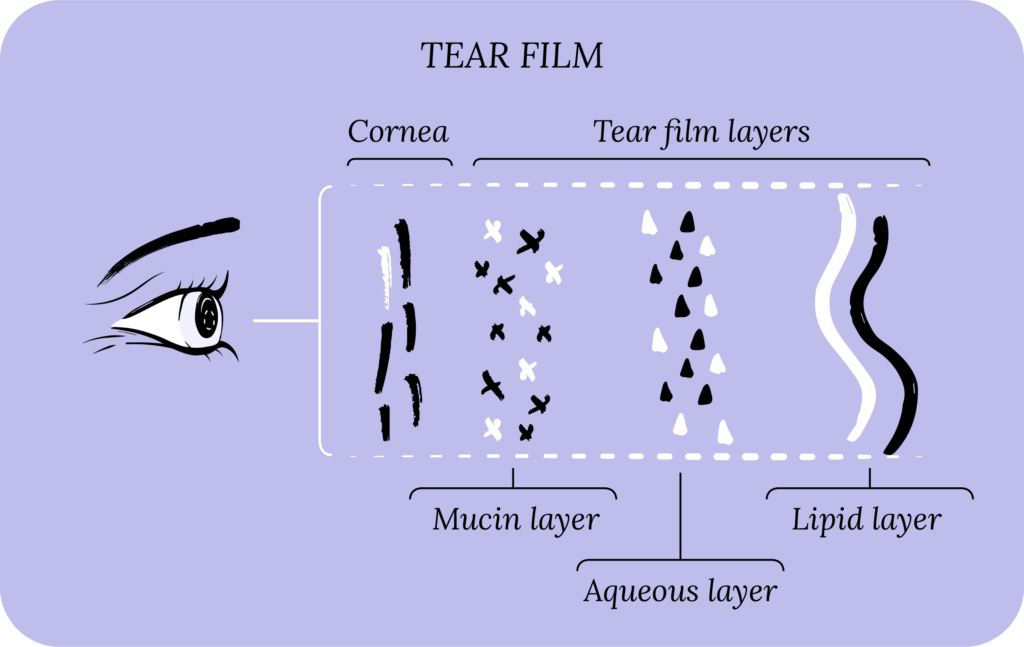
In MGD, meibomian oil glands malfunction and stop secreting oil, which leads to tear film instability and the onset of dry eye symptoms. Moreover, the oil can build up in the glands causing obstructions, leading to styes and inflammation (aka posterior blepharitis). Rosacea is another common cause of posterior blepharitis. On the other hand, anterior blepharitis is typically caused by bacteria, mites (Demodex), dandruff from your scalp and eyelashes (seborrheic dermatitis), allergies, and contact lenses.
MGD and blepharitis treatments start with eyelid hygiene (warm compresses and eyelid wipes). The warm compress improves meibomian gland function, and promotes oil secretion. The eyelid wipes clear any debris from backed-up oil, fend off inflammation, and may have antimicrobial properties. Eyelid hygiene protects you from the vicious cycle of MGD <–> blepharitis, while reducing inflammation, redness and puffiness, which leads to healthy eyelids and vibrant eyes.
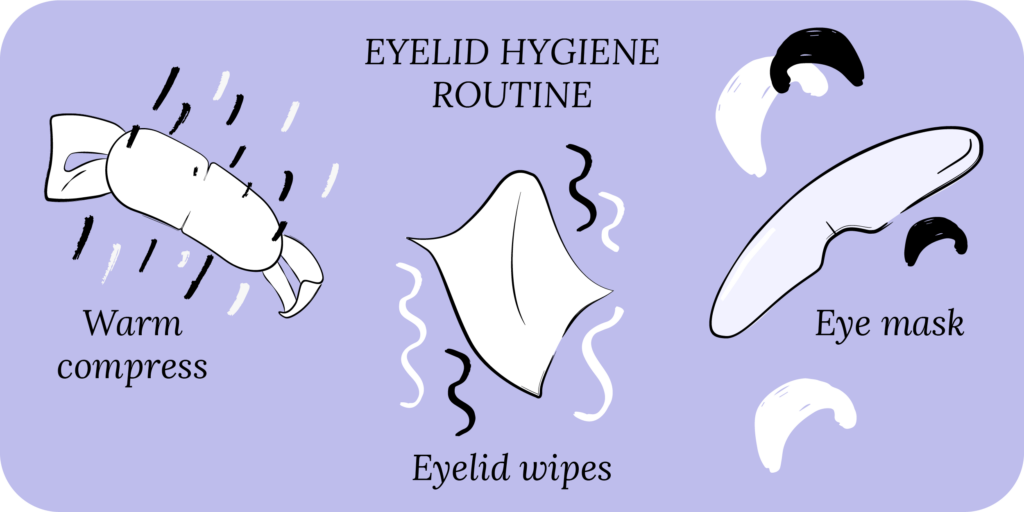
Thermal heating and eyelid cleaning
There are several procedures to treat MGD and blepharitis. Similar to the mechanism of warm compresses and eyelid wipes, most procedures for MGD and blepharitis either warm the meibomian glands or clean the eyelid margin and eyelashes. Typically after warming the eyelids, the liquified oil from the meibomian glands is expressed by pressure from a machine (probe) or by the eye doctor. This helps clear up any blockages and promotes healthy oil secretion.
Some procedures that include warming the eyelids and expressing the oil are LipiFlow®, iLux®, TearCare®, MiBo Thermoflo, OCuSOFT® Thermal 1 Touch™, eyeXpress™ Eye Hydration System.
Procedures that clean the eyelid margin and eyelashes include BlephEx® and NuLids™. Unlike other procedures, NuLids™ has been approved for at-home use, and patients can purchase it directly. Some eye doctors may also do an intensive eyelid cleaning in the office using a cleansing gel, such as I-Lid ‘N Lash® Pro, followed by a meibomian gland probing to “unclog” the glands and express the backed-up oil.

Rest
Warm Compresses
Perfect for eye dryness, fatigue, tearing, and puffiness of the eyelids. Free shipping 📦.
Try today - $30
Intense pulsed light
In addition to procedures for heating and cleaning the eyelashes, intense pulsed light (IPL) therapy is also used to treat MGD and blepharitis.5 IPL therapy has been widely used for skin conditions, but because of its properties to reduce inflammation and induce thermal heating, it has been adapted to dry eye treatment.
Without getting too technical, IPL uses different wavelengths of light, which determine the depth of penetration in and under the skin for the therapy. The longer the wavelength, the deeper the penetration. Along with depth, the wavelength is also specific for different tissues, such as skin (melanin) and blood vessels. The intensity of the light, the duration of the light energy pulse, and the time between subsequent pulses can also be varied. These parameters are varied depending on the desired area of treatment and a patient’s skin pigmentation (aka the Fitzpatrick skin types).
When light energy penetrates the intended tissue, it’s converted into heat energy, leading to a variety of therapeutic effects. In DED specifically, the heat can warm the meibomian glands, causing any backed-up oil to liquify and gland blockages to open. The heat can also ablate abnormal blood vessels, and prevent them from bringing pro-inflammatory markers to the eyelids. Lastly, the heat can promote synthesis of collagen and elastin in the eyelid skin, which may improve the overall structure and function of the eyelids.
Some procedures that employ IPL are LacryStim™ IPL, OptiLight®, Optima™ IPL, ThermaEyes® Plus IPL, and Epi-C-Plus®. While IPL is fairly specific for certain tissue, since it penetrates deeper than standard lasers, it may injure other tissue surrounding the site of therapy. Furthermore, IPL settings should be carefully adjusted to not damage melanin and cause skin changes.
Radiofrequency
Radiofrequency, like IPL, is contingent upon wavelengths, and the term “frequency” actually comes from the number of wavelengths per second.6 As with IPL, the wavelengths can penetrate tissue and cause heating, which may provide relief in DED related to MGD and blepharitis. TempSure® Envi is an example of a procedure that relies on radiofrequency.
Procedures for tear production and lubrication
In addition to procedures for MGD and blepharitis that address evaporative DED, there are procedures that can increase tear production and lubrication. The lacrimal gland, located in the orbit above the lateral part of the upper eyelid, is responsible for tear production. The lacrimal gland is connected to the lacrimal nerve. When the lacrimal nerve is stimulated, the lacrimal gland produces tears that lubricate the ocular surface. Just like the lacrimal nerve, the trigeminal nerve also plays a role in tear production.
Direct lacrimal nerve stimulation has only been performed in laboratory experiments on animals, and not people. Instead, some procedures and devices have been used on people to stimulate the trigeminal nerve, which can be accessed through the nose.7 TrueTear® (no longer in production) was a hand-held device that could stimulate branches of the trigeminal nerve in the nasal cavity. Production was stopped because patients found it uncomfortable putting the probe into the nose, and the cost of manufacturing the device was too high.
In 2020, the iTear® 100 device was approved for use in DED. Unlike TrueTear, which is inserted into the nose, iTear® 100 can stimulate branches of the trigeminal nerve on the external surface of the nose.
In addition to tear production, Lacrisert® is an at-home procedure which provides continuous lubrication to the ocular surface. Lacrisert® is a small water-soluble insert made of hydroxypropyl cellulose. You may recognize this ingredient because it or related versions are in your typical artificial tears. The Lacrisert® is inserted into your inferior fornix (the pocket between your eyeball and lower eyelid), and as it dissolves, it provides lubrication.
Corneal healing procedures
In addition to procedures that treat the causes of evaporative or aqueous deficient DED, there are other options that address the surface of the cornea directly. In moderate to severe cases of DED, soft scleral lenses or rigid lenses may provide relief. These lenses work by trapping tears between the lens and the cornea, thereby providing it with constant lubrication.
In severe cases, or when significant inflammation is present, amniotic membranes may be a good option.8 Amniotic membranes are derived from the human placenta, and reduce inflammation and promote tissue healing. Some amniotic membranes can be placed on the cornea in the office, while others require surgery.

Rescue
Cold Compresses
Perfect for sudden flare-ups of eye dryness, pain, burning, and swollen/inflamed eyelids. Free shipping 📦.
Try today - $12
Eyelid and conjunctival surgery for dry eyes
In some instances of severe chronic DED, surgery may be considered. As mentioned above, one option is to do an amniotic transplant on the conjunctiva (the clear membrane that lines your eyeball). In cases where eyelashes are touching and irritating the cornea, the eyelashes can be removed using forceps (epilation). However, this is typically a short-term solution, and in patients with chronic eyelash misdirection, cryotherapy (freezing the eyelash follicles), or surgery may be considered. Surgery may also be an option in cases where the eyelids don’t properly appose the globe, causing tears to run down your cheek, leading to dry eyes. Finally, the eyelids can be temporarily closed to allow for corneal healing. This is generally reserved for very severe cases where the patient is rapidly worsening.
In patients with redundant conjunctiva (conjunctivochalasis), the tear film may become disrupted and unable to properly coat the ocular surface. This redundant conjunctiva can be removed, and an amniotic transplant may be used to allow the remaining conjunctiva to heal while reducing inflammation.
Cost and availability of common procedures for dry eye treatment
While procedures may be a good option for some patients, the cost and availability can be a limiting factor. Most procedures and devices for dry eye treatment are not typically covered by insurance. Punctal plugs, amniotic membrane placement or transplant, and some reconstructive (not cosmetic) surgeries are typically covered. But even these may require additional paperwork from your eye doctor and multiple calls to your insurance company.
Depending on where you live in the country, the typical out-of-pocket cost for procedures not covered by insurance can range from $500 – $1,500 per treatment. Moreover, patients will often require multiple treatments to see results, which can multiply the total costs. This lack of price predictability and transparency for these procedures is frustrating and costly for patients.
The availability of these procedures is limited as most eye specialists don’t have the necessary equipment. While the internet has made it easier to locate nearby eye doctors who perform these procedures, patients may still have to travel long distances for treatment.

All Rounder
Eyelid Hygiene Plan 3
Perfect for eye dryness, burning, itching, grittiness, crusting/flaking of eyelashes and inflamed/swollen eyelids. Free shipping 📦.
Try today - $60
What’s in the pipeline
There are approximately 5-10 new procedures and devices that are currently being studied and may be available for use in the near future. Neurostimulation is a hot topic, and new devices may allow for direct stimulation of the lacrimal nerve, along with better stimulation of the trigeminal nerve. Similarly, transcutaneous electrical nerve stimulation is being studied to mitigate the pain experienced in DED. Many other devices in development are addressing rapid tissue healing and reducing ongoing inflammation. These new procedures will provide more options for patients, but the above-mentioned barriers will likely still be a factor, namely cost and availability.
Putting it all together
Procedures and devices provide patients with another option for dry eye treatment. These procedures and devices typically focus on five major categories:
- Tear drainage system
- Meibomian gland dysfunction and eyelid inflammation
- Tear production and lubrication
- Corneal healing
- Eyelid and conjunctival surgery
While procedures may be a good option for some patients, cost and availability can be limiting factors. Moreover, many patients turn to procedures as a “magic” cure, only to be dissapointed. Like with prescriptions, dry eye treatment procedures work best when used in conjunction with a good overall treatment plan that includes eyelid hygiene, artificial tears, good nutrition and hydration, and important lifestyle changes. Your eye care and eye health reflect your overall general health, and what’s good for the eyes should also be good for the mind and body.
What’s next
We really think everyone should take our Dry Eye 101 course. Find it here!
If you’ve already taken it, amazing! Check out more articles in the Continuing Education section below.