What is Dry Eye Disease?
If you’re reading this article, either you or someone you know has dry eye disease (DED). So what is dry eye disease? Dry eye disease, also called dry eye syndrome, is a chronic condition that affects millions of people worldwide, and can impact you on multiple levels.
In addition to your eye health, DED can influence your physical and mental well-being. Once you have DED, your symptoms may come and go, but you will typically have it for the rest of your life. We know this seems daunting, but with a good treatment plan you can take control of your DED!
This article will answer the question “What is Dry Eye Disease?” and help you understand the causes, symptoms, and treatment options for DED.
Key Points
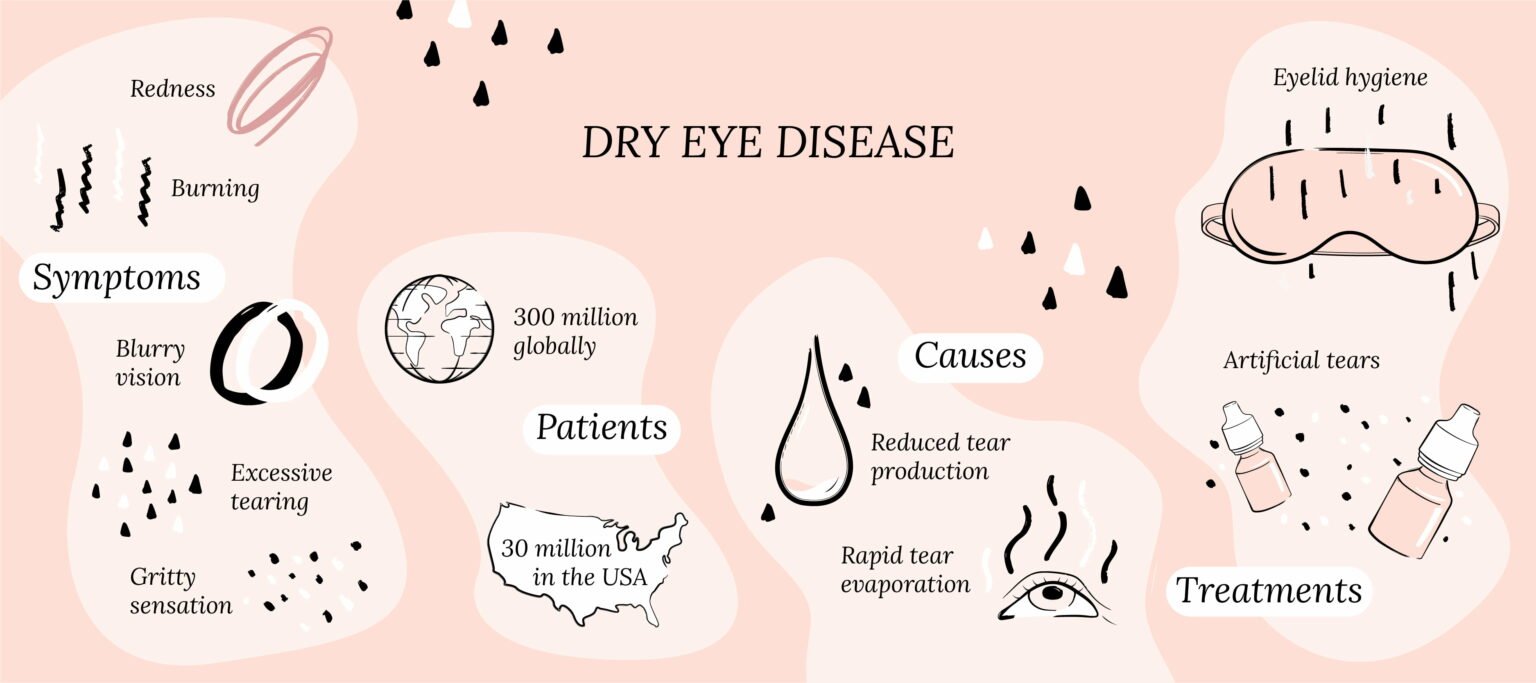
- Dry eye disease is a chronic condition that affects 30 million Americans and 300 million people worldwide.
- In addition to eye symptoms, dry eye disease can affect your physical and mental well-being.
- Dry eye disease is chronic but can be treated.
What is Dry Eye Disease?
Dry eye disease (DED) is also known as dry eye syndrome, keratoconjunctivitis sicca and ocular surface disease. DED is a chronic condition caused by unstable tears and inflammation, and leads to symptoms such as redness, burning, irritation, gritty sensation and blurry vision.
The Tear Film & Ocular Surface Society Dry Eye Workshop II defines DED as “a symptomatic disease, characterized by a vicious cycle of tear film instability and hyperosmolarity, which leads to increased ocular surface inflammation, damage and neurosensory abnormalities.”1
Your tear film coats the front part of your eyes called the cornea, and plays a crucial role in protecting your eyes, making them feel comfortable, and helping you see clearly. With dry eye disease, your tear film doesn’t work as it should, which sets off a cascade of inflammation, leading to symptoms.
Who Gets Dry Eye Disease?
Literally everyone. If you’re reading this, chances are that you or someone you know has DED. Approximately 30 million Americans, and over 300 million people worldwide are affected by it.1 But the actual number is probably much higher. In fact, one in every three eye care clinic visits is related to symptoms of dry eyes.2
Think about it, anyone looking at a computer or phone screen (basically all of us these days!), doing tasks that require long focus without blinking, such as driving, living in high pollution and low humidity areas, will get dry eye symptoms. When these symptoms occur often and get in the way of your life, that’s when you have DED.
The Impact of Dry Eye Disease
Dry eye disease is tough. While it doesn’t cause blindness, DED puts you at risk for vision-threatening complications, such as corneal infections and scarring. DED can have a significant impact on your life, leading to social, emotional and financial burdens.3 You may suffer from symptoms for months, try several over-the-counter treatments, and spend a lot of time, energy and money before seeking professional help.

Rest
Warm Compresses
Perfect for eye dryness, fatigue, tearing, and puffiness of the eyelids. Free shipping 📦.
Try today - $30
You may see multiple eye doctors because you feel they’re not taking you seriously, or spending enough time listening to you. This is not the eye doctor’s fault. Taking care of DED requires more time with the patient, which is not always possible in a busy practice with overhead expenses. As you can imagine, this leads to frustration, hopelessness, and treatment failure.4
DED is manageable and treatable, just like other chronic conditions that affect the body, such as diabetes and high blood pressure. We’re here to get you the best treatment and support as soon as you have symptoms. At CorneaCare, we specialize in dry eye disease and have honed our craft and our workflow so we can spend time listening, supporting, and providing you with personalized eye care.
Our Community
Chat, share, and learn from our doctors, coaches and others like yourself
👩⚕️ Get answers!
Having DED should not prevent you from doing anything you love or need to do. With consistent effort on your part and the right support, you can protect and preserve your eyes, and live a healthy, fun, and prosperous life.
What Are the Symptoms of Dry Eye Disease?
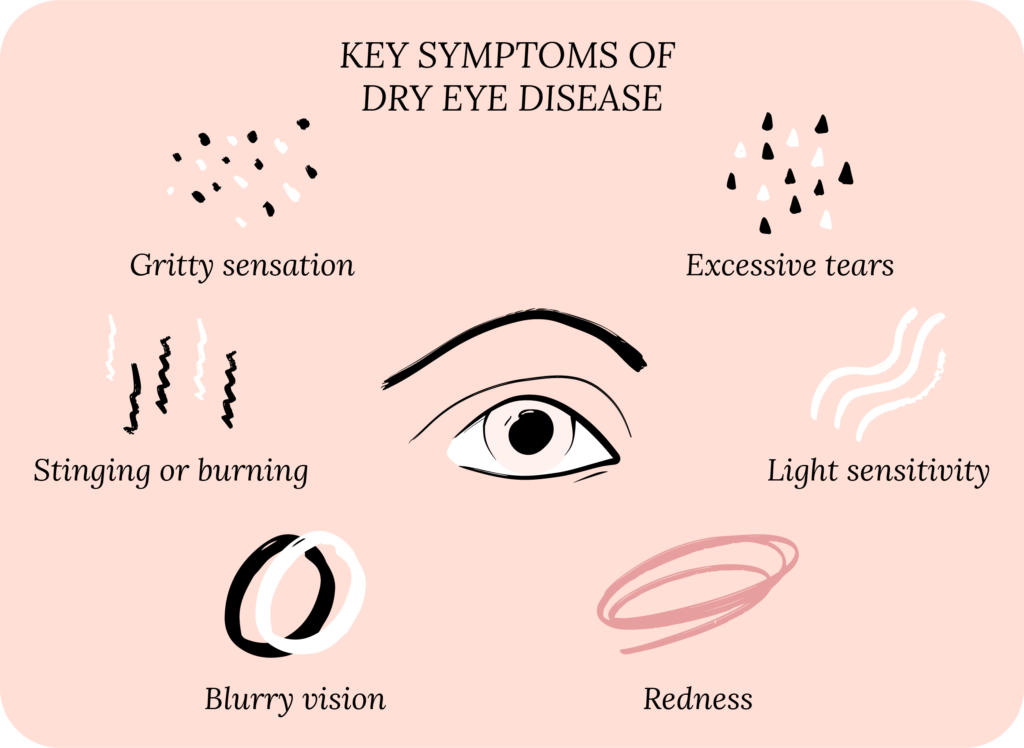
Everyone experiences dry eye symptoms differently. Your own experience with DED is very important to us, but the typical symptoms are:5
- Redness
- Pain
- Irritation
- Gritty feeling, or foreign body sensation
- Dryness
- Blurred vision
- Tearing or watery eyes
- Burning or stinging of the eyes
- Light sensitivity
- Eye fatigue
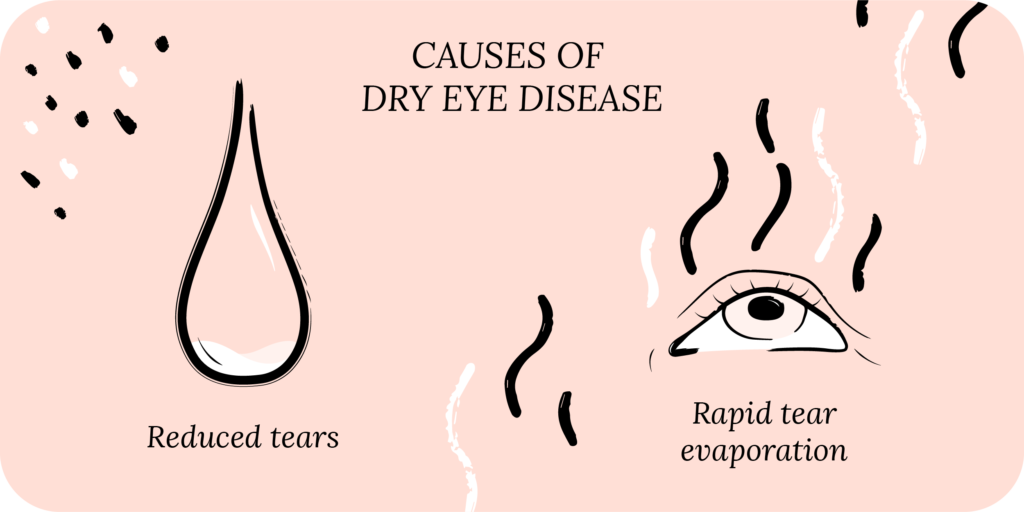
What Are the Causes of Dry Eye Disease?
Dry eye disease is not your fault! The best way to think about what causes DED is to divide it up into decreased production of tears (aqueous deficient) or rapid evaporation of tears (evaporative).1
Decreased Tear Production
Your natural tears are produced by the lacrimal gland. Infection and inflammation may cause the lacrimal gland to malfunction, leading to decreased tear production.
One cause of inflammation of the lacrimal gland is Sjögren’s syndrome, an autoimmune condition, which is typically associated with severe dry eyes. Another cause of less tear production is a problem with the link between the cornea and the lacrimal gland. When the cornea is dry, it naturally alerts the lacrimal gland to produce more tears. If this doesn’t work, tear production may decrease. This is often seen in people who have had eye injuries, infections or surgeries that decrease the sensitivity of the cornea.

Rescue
Cold Compresses
Perfect for sudden flare-ups of eye dryness, pain, burning, and swollen/inflamed eyelids. Free shipping 📦.
Try today - $12
In addition to decreased tear production, you could have increased tear evaporation, which also leads to dry eyes.
Increased Tear Evaporation
Your tear film is made up of three layers: the mucin layer, the aqueous layer and the lipid layer. The mucin layer is made up of molecules that allow it to bind to the surface of the cornea. The aqueous layer then sits on top of the mucin layer, and the lipid layer sits on top of the aqueous layer.
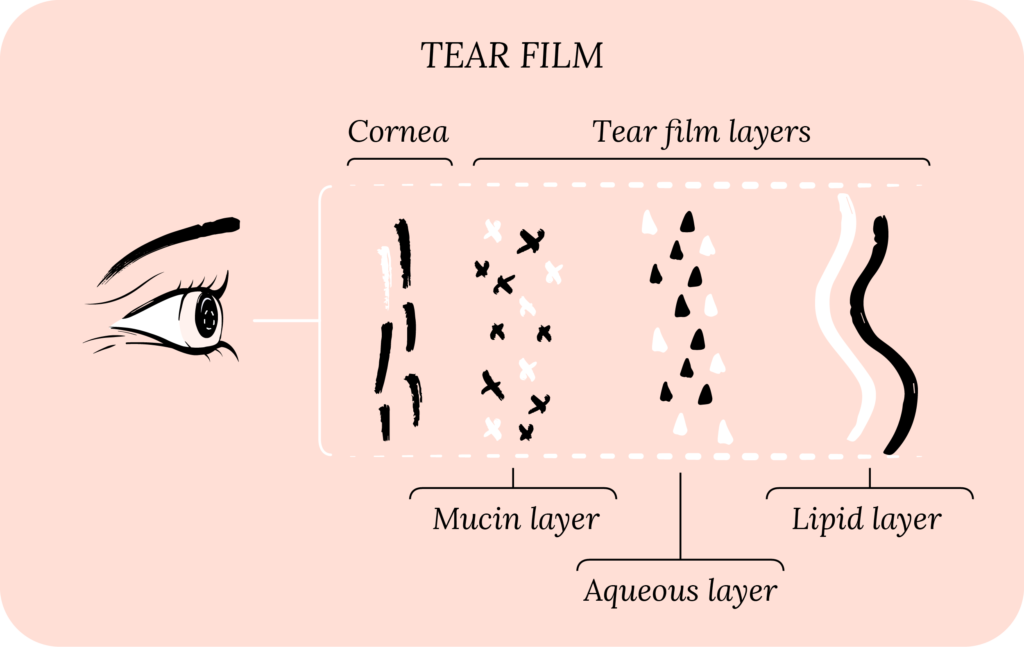
All three of these layers work together to stabilize the tear film and prevent tear evaporation.
If the surface of the cornea is damaged, it may not bind to the mucin layer well. Or if there is a decrease in the oil production for the lipid layer, such as in meibomian gland dysfunction, your tear film may not be stable.
Contact Lenses
Contact lens use is another common cause of DED. This is because contact lenses may directly lead to changes on the cornea or decrease the sensitivity of the cornea, leading to symptoms of chronic dry eye.
Risk Factors for Dry Eye Disease
Eye surgery, specifically refractive surgery (LASIK), and preexisting eye conditions, such as corneal diseases and glaucoma, are risk factors for DED. Additional risk factors for dry eye syndrome include:6
- Age above 50 years old
- Female gender
- Medications such as oral antihistamines, antidepressants, decongestants, diuretics or birth control pills
- Hormonal changes due to menopause
- Autoimmune diseases including thyroid eye disease and rheumatoid arthritis
- Medical conditions such as cancer and diabetes
- Poor nutrition (low vitamin A)
- Environmental factors (high pollution or low humidity)
- Occupational factors (prolonged use of computer screens)
How Dry Eye Disease is Diagnosed
There are several ways to diagnose dry eye disease, but it all starts with listening to you, the patient.6 In fact, there are instances when a patient has classic symptoms without any abnormal exam findings.7
Several questionnaires can be used to assess your symptoms. For example, the Ocular Surface Disease Index (OSDI), the Standard Patient Evaluation of Dry Eye Questionnaire (SPEED), or the Dry Eye Questionnaire (DEQ). These surveys attempt to capture your personal experience with dry eye disease as data your doctor can use.8
Rise
Eyelid Wipes
Perfect for eye dryness, itching, burning, and crusting/flaking of eyelashes. Free shipping 📦
Try today - $25
What to Expect During an Eye Exam for Dry Eye Disease
During your exam, your eye doctor (optometrist or ophthalmologist) looks at the skin around your eye, your eyelids, and eyelashes, and how you blink.
If the skin around your eye is red, you may have rosacea and signs of blepharitis (inflammation of the eyelids). On your eyelids, your doctor looks for signs of meibomian gland dysfunction. When you blink, if part of your eye is still open (incomplete blink), your doctor considers eyelid function.
Your eye doctor also examines the surface of the cornea, the tear film, and the conjunctiva (thin membrane inside your eyelids and covering the white of your eye, the sclera).
On the surface of the cornea, they check for corneal sensation, corneal staining, tear film break-up time (TBUT), and tear production over 5 minutes. Corneal sensation is typically checked with a cotton tip application (q-tip).
Your eye doctor may use a dye called fluorescein to stain the surface of your cornea and conjunctiva, highlighting areas where the surface is loose, not as strong, or broken off. Fluorescein also helps measure TBUT, an indicator of tear film stability. The faster your tear film breaks up, the quicker your tears evaporate.
Finally, your optometrist or ophthalmologist may perform the Schirmer’s test, where a strip is placed gently on the inside of your eyelid to measure how many tears you produce over 5 minutes.
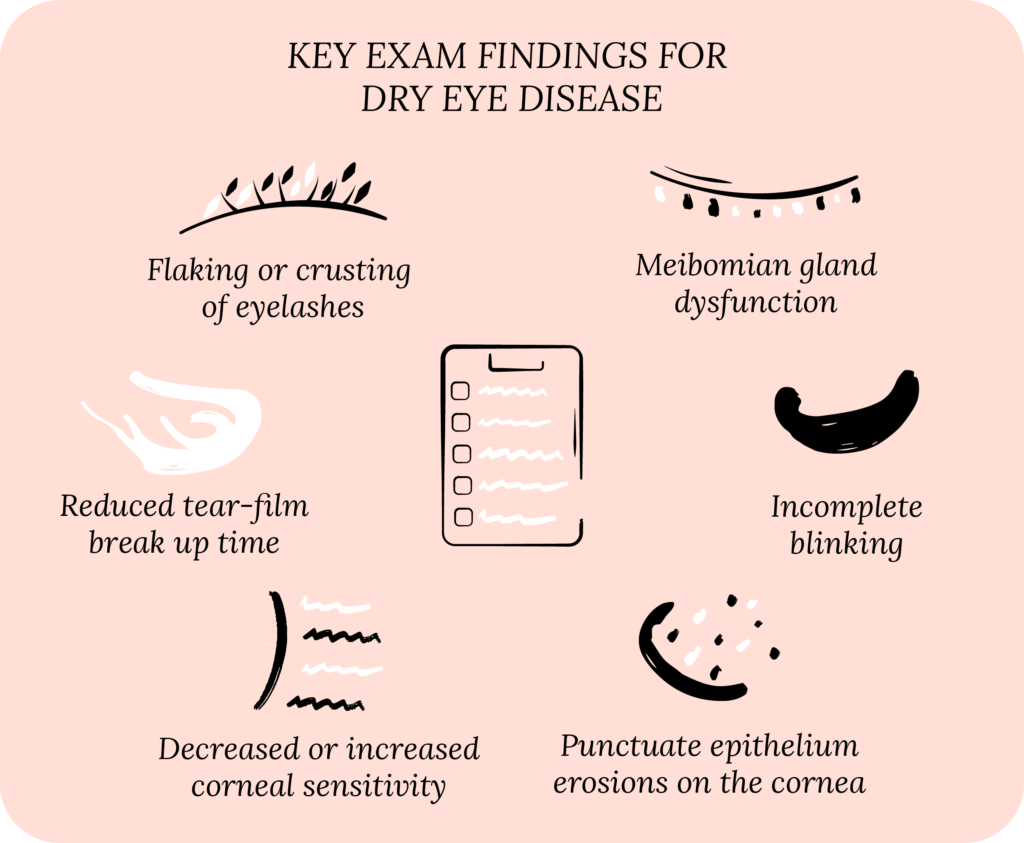
Other tests for inflammation and tear osmolarity measurement can determine the concentration of various molecules in your tears. High-quality imaging measures the height of the tear meniscus, tear film quality, and thickness of the lipid layer.
How Dry Eye Disease is Treated
Unlike what you may have heard, dry eye treatment is not as simple as using eye drops. Remember dry eye disease is chronic, and therefore treating DED requires continued effort on your part.9 But no worries, we’re here to support you at each step!
Treatment options for dry eye syndrome can be divided into five components:
- Education, implementation, and consistency
- Tear replacement
- Prevent tear evaporation
- Reduce inflammation
- Promote healthy nerve function and growth
The most important aspect of treatment is learning about dry eye disease, implementing a treatment plan, and staying consistent. Knowledge is power, and learning about DED is the first step to living well with DED.
Once you have a treatment plan, you have to implement it so that it integrates into your daily routine, and becomes habitual. Lastly, you have to stay consistent. You can have the best treatment, but if you do not stick to it consistently, it won’t work.10

All Rounder
Eyelid Hygiene Plan 3
Perfect for eye dryness, burning, itching, grittiness, crusting/flaking of eyelashes and inflamed/swollen eyelids. Free shipping 📦.
Try today - $60
Artificial Tears and Eyelid Hygiene
To treat the aqueous deficient type of dry eye disease (not making enough tears), we can replace the deficiency with artificial tears to improve lubrication on the surface of the eye. There are over 50 different types of artificial tears. They can contain preservatives or be preservative-free, with different viscosities (thickness) and come in bottles or individual vials. You can also do tear replacement therapy with gels and ointments, which are used at bedtime.
To treat the evaporative type of dry eye syndrome, we can prevent tear evaporation. To accomplish this, we implement an eyelid hygiene routine with warm compresses and eyelid wipes. The goal is to optimize meibomian gland function, and produce a good lipid layer to prevent your tears from evaporating. There are many in-office procedures that heat and massage the meibomian glands.
Other in-office procedures include punctal plugs, which block the tear ducts to allow tears to stay in your eyes longer. Several prescription eye drops are coming to market that address eyelid hygiene.
Most individuals will have features of both aqueous deficient and evaporative DED. Therefore, a treatment regimen often consists of lubrication and eyelid hygiene.
Treating Inflammation
We know inflammation plays a vital role in dry eye syndrome. Therefore, reducing inflammation is an important part of treatment. We typically do this with anti-inflammatory prescription eye drops, such as steroids, cyclosporine (Restasis and Cequa) and lifitegrast (Xiidra). Another approach is to eat food rich in anti-inflammatory compounds and antioxidants, such as Omega-3 fatty acids.
Here at CorneaCare, we stress the importance of your diet. Eating a well-balanced diet, with anti-inflammatory and antioxidant properties, is not only good for your eyes, but also foundational for your mind and body.
About Cornea Nerve Function
Promoting healthy nerve function and nerve growth in the cornea is not well understood, but we know it is important. The nerves in your cornea help with sensation (temperature, touch, pressure and pain), and stimulate your lacrimal gland to produce tears. Inflammation and changes in tear osmolarity (concentration) can cause damage to the nerves in the cornea. If the nerves get damaged, they may not communicate with the lacrimal gland, and alert it to produce tears.
Alternatively, the nerves can become hypersensitive, causing them to activate randomly, or become overactive to mild stimuli. Meaning that a patient with seemingly “normal” eyes during an exam may still experience severe symptoms because the corneal nerves are hypersensitive.
Remember what we said – your experience with DED is just as important as the clinical exam. You can learn more about the treatment options for DED.
Putting It All Together
CorneaCare is here to give you a voice and listen to you. Dry eye disease is physically and emotionally exhausting. We know you have been through difficult times searching for answers and trying to find treatments that work.
We do not believe in creating one-sided physician-to-patient treatment plans. That would just perpetuate what is already wrong with DED treatment. These are your eyes we’re talking about, and you should be in the driver’s seat for making treatment decisions, with our support. We want to empower you to take control of your dry eye disease.
What’s Next:
Let’s dive into the different types of dry eye disease.