Choosing the Best Prescription Eye Drops for Dry Eyes
We get it! Dry eye treatment can be daunting. Using artificial tears multiple times a day, the eyelid hygiene routine and the lifestyle changes add up. Without guidance and motivation, it’s difficult to stick to a dry eye treatment regimen, even if it may be working. Many patients end up turning to prescription eye drops for dry eyes as a “magic cure.” Many eye doctors (ophthalmologists and optometrists) also turn to prescription drops, partly because of patient preference, and partly because counseling patients on treatment compliance and lifestyle modifications takes time and effort, which isn’t always available in a busy clinical practice.
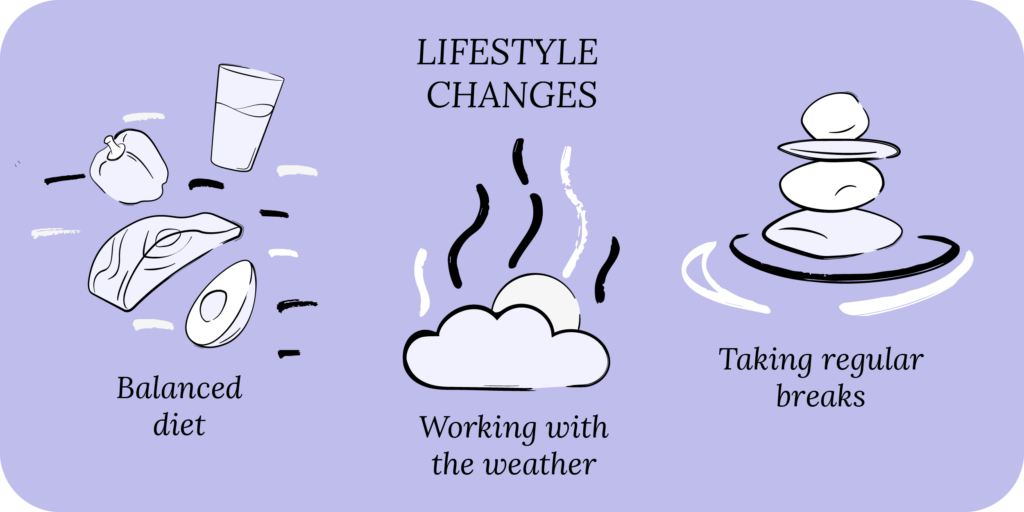
While prescription eye drops can certainly help, they work best as a supplement to, and not a replacement for, a well-rounded dry eye treatment regimen, including over-the-counter eye drops, eyelid hygiene, healthy diet, drinking lots of water and living a healthy lifestyle. Your eye care is linked to your healthcare, so what’s good for your mind and body is also good for your eyes.
Key points
- Several prescription eye drops for dry eyes are currently available, and they may be a good option for select patients.
- Dry eye prescription drops work best when used alongside eyelid hygiene, eye lubrication and lifestyle changes.
- Most dry eye prescription drops are expensive and require prior authorization from insurance, which makes it difficult to obtain coverage for some patients.
dry eyes seriously?
Dry Eye Disease
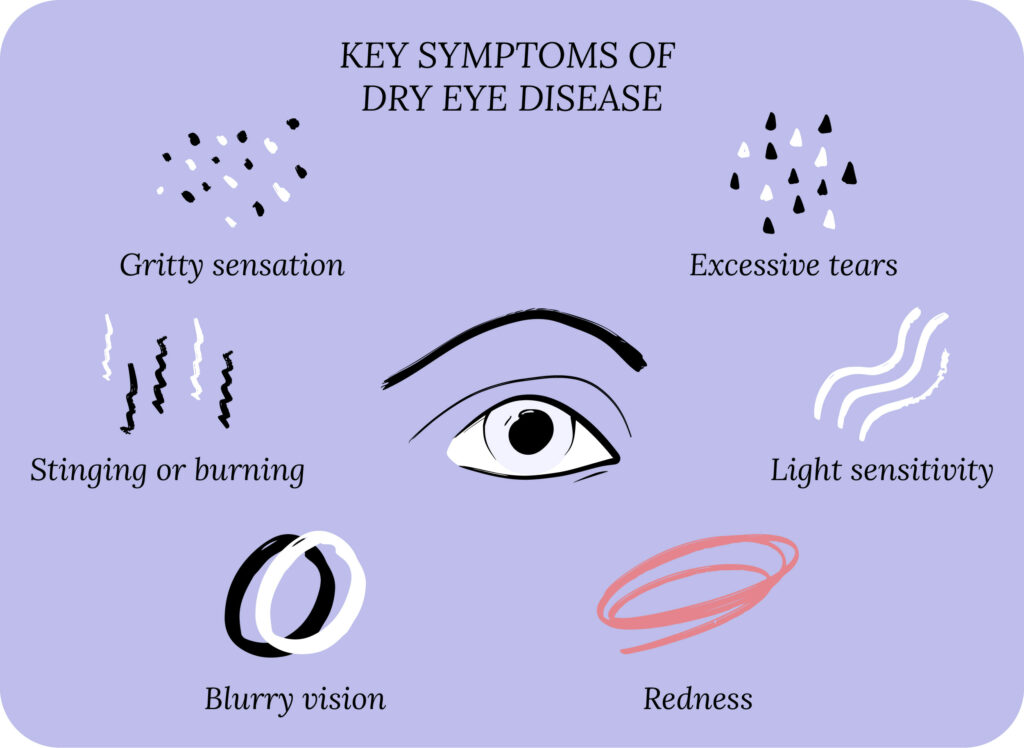
Before discussing prescription eye drops for dry eyes, let’s cover some dry eye basics. Dry eye disease (DED) can also be referred to as dry eye syndrome, keratoconjunctivitis sicca and ocular surface disease.1 The typical symptoms of dry eye are blurry vision, gritty sensation, itchy eyes, light sensitivity, excessive tearing, dryness, burning sensation, and red eyes.
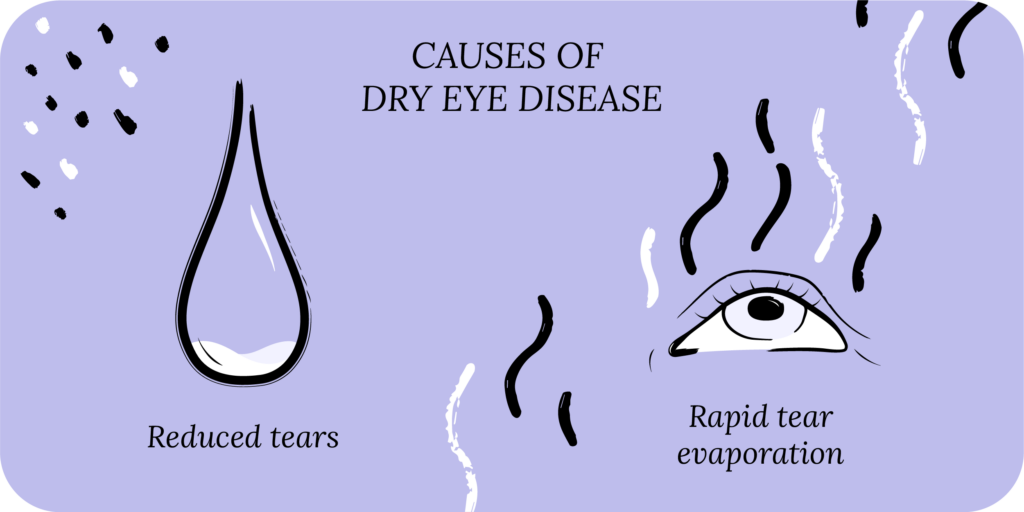
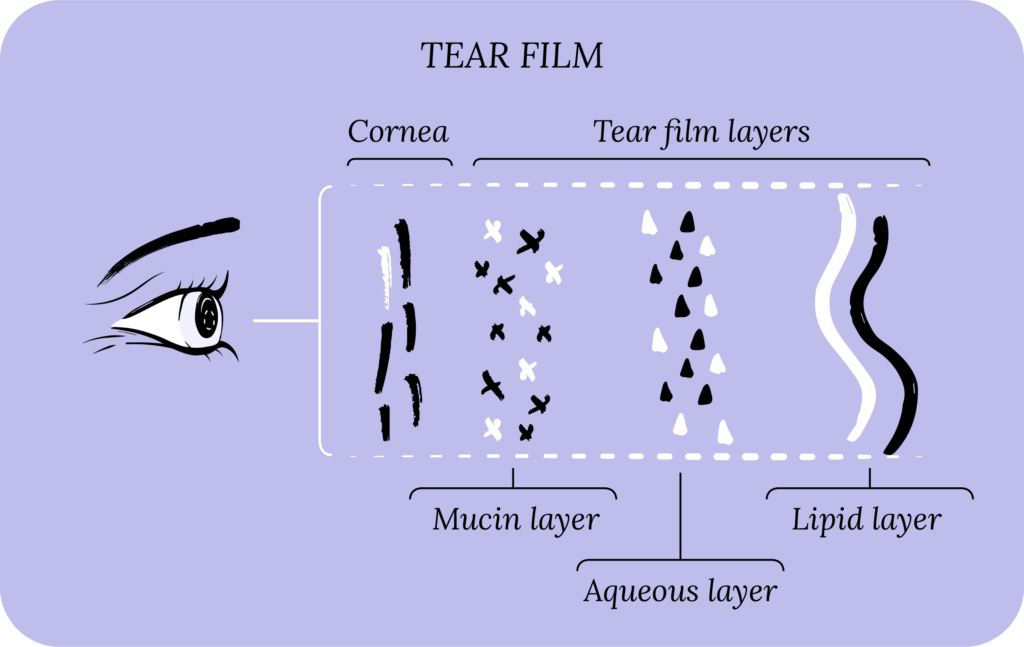
There are two major classes of DED: aqueous deficient and evaporative. In aqueous deficient DED, your body doesn’t produce enough natural tears to lubricate the ocular surface (the cornea and conjunctiva). In evaporative DED, your tear production is normal, but the tears evaporate too quickly. Evaporative DED is far more common than aqueous deficient, and most patients typically have a mix of both, leading to tear film dysfunction.
Pre-existing eye conditions, such as meibomian gland dysfunction (a problem with oil glands in the eyelids), blepharitis (eyelid inflammation), glaucoma and eye surgery can predispose you to DED. Oral medications, such as antihistamines, antidepressants, birth control pills, decongestants, and beta blockers are risk factors for DED. Medical conditions, such as Sjögren’s syndrome, rheumatoid arthritis, menopause, diabetes and high blood pressure can also contribute to dry eye symptoms.
Dry climate (low humidity), high winds, air pollution and air allergens can worsen dry eye symptoms. Lifestyle risk factors for dry eye include extended use of digital screens, wearing contact lenses, poor diet, and smoking.
DED can affect your physical, emotional, financial and even social wellbeing. It’s therefore important to start a dry eye treatment plan to get dry eye relief and prevent long-term complications and eye problems.
Dry Eye Treatment
A good way to approach dry eye treatment is to think of the causes of dry eyes. For aqueous deficient DED, lubricating eye drops can augment your tear film and make up for decreased tear production. For evaporative DED, eyelid hygiene can stabilize your tear film and prevent rapid tear evaporation.
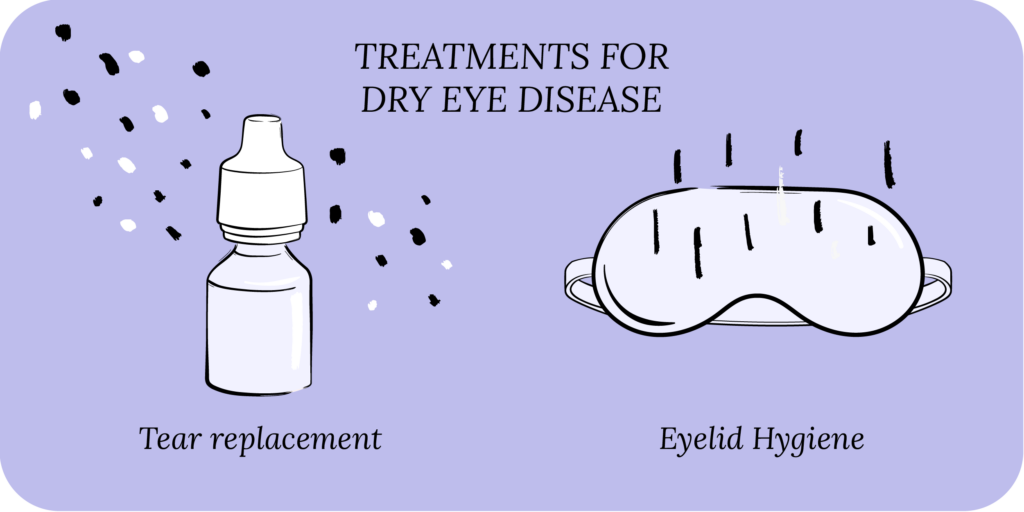
The treatment options for dry eye include eye drops (artificial tears), gels, ointments and eyelid hygiene (warm compresses and eyelid wipes). Drinking lots of water and eating a well-balanced diet (vitamins, minerals and fatty acids) can help, as can taking an oral dry eye supplement. In some cases of severe dry eyes, a person may require prescription eye drops, oral prescription medications, and in-office ophthalmic procedures.

Foundation
Eyelid Hygiene Plan 2
Perfect for eye dryness, burning, itching, crusting/flaking of eyelashes and inflamed eyelids. Free shipping 📦.
Try today - $45
Prescription Eye Drops for Dry Eyes
Pharmaceutical companies have made significant progress in developing new treatments for DED.2 Several drugs have already been approved by the Food and Drug Administration (FDA) for DED, and many more are in the pipeline. These drugs can be prescribed by ophthalmologists and optometrists (in most states), and are not available over the counter (OTC).
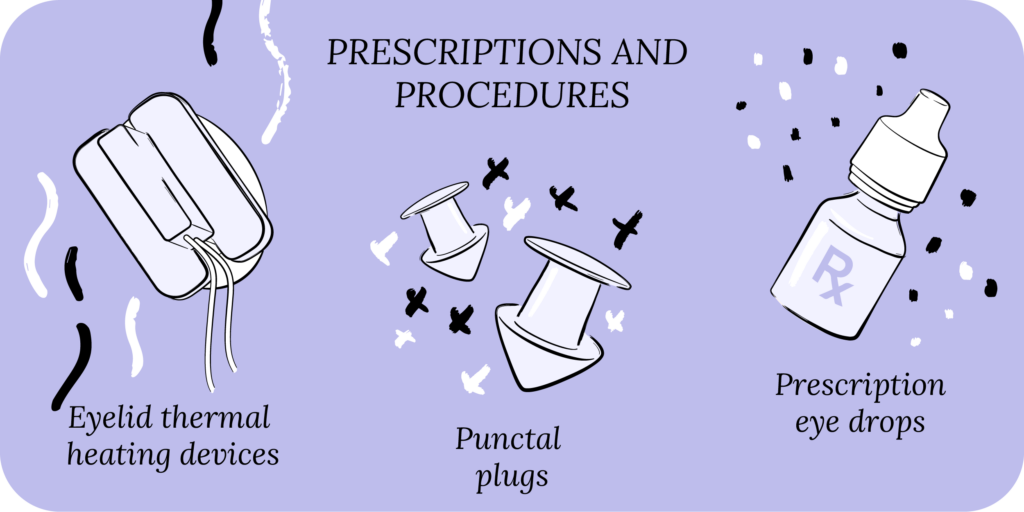
Most dry eye prescriptions focus on four major categories: reducing inflammation, increasing tear production, stabilizing the tear film, improving corneal nerve function and strengthening the corneal surface. In the sections below, we’ll cover some of the major prescriptions available for dry eye patients.
While prescriptions for DED can be an option for select patients, there are two main issues. One, prescriptions are not a “magic cure,” and work best when combined with an overall treatment plan that includes artificial tears, eyelid hygiene, nutrition and lifestyle. And two, many insurance providers will not cover DED prescription medications without prior authorizations, which can make it difficult to obtain coverage for some patients.
Cyclosporine
Cyclosporine primarily works as an anti-inflammatory agent, but may also increase tear production and the development of goblet cells in your conjunctiva.3 Goblet cells release mucin, which plays an important role in stabilizing your tear film and anchoring it to the cornea. By reducing inflammation and improving tear film stability, cyclosporine may help with dry eye symptoms.
Restasis® is cyclosporine 0.05% (Allergan) and CequaTM is cyclosporine 0.09% (SUN Ophthalmics). Both typically come in individual preservative-free vials, but Restasis® has also recently released a multi-dose preservative-free bottle. Klarity-C® is cyclosporine 0.1% (ImprimisRx), a compounded drop, and comes in a multi-dose preservative-free bottle. It’s unclear whether one concentration of cyclosporine works better than the other, but they all tend to be tolerated similarly by patients.
The most common side effect of cyclosporine is burning, redness, itchiness, foreign-body sensation, tearing, stinging and light sensitivity. Some patients may put these drops in the refrigerator, or use an artificial tear before the prescription drop to minimize the side effects.
If you don’t have insurance, or your insurance doesn’t cover these prescriptions, the average out-of-pocket cost is around $600 per month for Restasis® and CequaTM. The FDA recently approved a generic cyclosporine 0.05%, which may increase the availability of this drug for more patients.

Rest
Warm Compresses
Perfect for eye dryness, fatigue, tearing, and puffiness of the eyelids. Free shipping 📦.
Try today - $30
Lifitegrast
Lifitegrast is an anti-inflammatory agent.4 While cyclosporine modulates your inflammatory cells, lifitegrast blocks them from activating, which reduces the secretion of molecules that cause inflammation. Xiidra® is lifitegrast 5.0% (Novartis) and is available as individual preservative-free vials.
The main side-effects of lifitegrast are the same as cyclosporine, namely burning, redness, itchiness, foreign-body sensation, tearing, stinging and light sensitivity.
Without insurance coverage, the out-of-pocket cost of Xiidra® is around $600 per month.
Varenicline
Varenicline is the new kid on the block, and was approved by the FDA in October 2021 for use in DED.5 Unlike cyclosporine and lifitegrast, varenicline comes as a nasal spray, and acts on your nervous tissue to increase tear production. TyrvayaTM is varenicline 0.03mg. Common side effects include sneezing, coughing, and nose and throat irritation.
Without insurance coverage, the out-of-pocket cost of TyrvayaTM is around $600 per month.
Our Community
Chat, share, and learn from our doctors, coaches and others like yourself
👩⚕️ Get answers!
Steroid Eye Drops
Steroid eye drops primarily work by decreasing inflammation.6 We typically use them for a short course because steroids can increase the pressure in the eye predisposing you to glaucoma. Further, they can cause cataract formation and progression. Steroids work well in severe dry eyes to break the cycle of inflammation and provide relief while the patient gets accustomed to more long-term treatment (eyelid hygiene and artificial tears). Steroids also work well where a quick improvement in dry eyes is needed, such as before cataract and refractive surgery.
There are various low potency (strength) steroid solitons, suspensions and ointments available for dry eyes. Commons ones will contain loteprednol, fluorometholone and prednisolone. For example, Eysuvis® is loteprednol 0.25% (Kala Pharmaceuticals) and is approved for acute DED exacerbations and flare-ups. Some of the other steroid drops may be available as generics. However, several of the low concentration steroids are brand name and can be costly without insurance coverage.

Rescue
Cold Compresses
Perfect for sudden flare-ups of eye dryness, pain, burning, and swollen/inflamed eyelids. Free shipping 📦.
Try today - $12
Antibiotics
Antibiotics can play an important role in dry eye treatment.7 In addition to fighting pathogens, certain antibiotics can help reduce inflammation and strengthen the corneal surface. Tetracyclines, such as doxycycline, can have potent anti-inflammatory effects when used at low doses. They can help treat conditions that cause or worsen DED, such as rosacea.
Azithromycin can help fend off bacteria that cause blepharitis (eyelid inflammation), which is a risk factor for DED. Both doxycycline and azithromycin may also improve the overall structure of the cornea.
Oral forms of these antibiotics are relatively inexpensive, but getting topical versions suitable for the eyes can be expensive. Topical azithromycin is available as AzaSite®, while topical doxycycline has to be specially made at a compounding pharmacy.
Options also include antibiotic + steroid combination drops or ointments, which can amplify the antimicrobial and anti-inflammatory effects.

All Rounder
Eyelid Hygiene Plan 3
Perfect for eye dryness, burning, itching, grittiness, crusting/flaking of eyelashes and inflamed/swollen eyelids. Free shipping 📦.
Try today - $60
Secretagogues
Secretagogues are agents that promote the secretion of other compounds. For example, we use oral secretagogues in type II diabetes to promote the release of insulin, which controls blood sugar. Likewise, secretagogues can be used to increase the secretion of aqueous and mucin layers to stabilize your tear film.
Oral secretagogues include pilocarpine, but its use is limited because of adverse side-effects (excessive sweating and stomach problems). Secretagogue drops are available in Asian countries, but not in the US.8
Corneal Nerve Function and Dry Eye Disease
Recent literature has highlighted that dry eye disease may be related to how your body processes pain.9 The eyes sense pain through nerves in the ocular surface, namely the cornea. In DED, these corneal nerves may be overly sensitive and cause you to experience pain even without any stimulus. Therefore, improving corneal nerve function may help alleviate some of the symptoms of dry eyes.
This is an active area of research, and we will likely see new therapeutics in the future to address this new approach to treating DED.
Compounded Eye Drops and Ointments
Aside from prescriptions, many drugs can be compounded as drops or ointments at specialty pharmacies to provide dry eye relief in severe cases.10 These include vitamin A, N-acetylcysteine, serum tears, albumin tears, hormones, and tacrolimus. All of these will require a prescription from your eye doctor, and prices may vary depending on insurance coverage.
How to Use Prescription Eye Drops
We have previously discussed how to properly use eye drops, gels and ointments. The key things to remember are cleanliness (don’t touch the tip with your hands or touch the tip to the surface of your eye), tilt your head back for drops, and generally use ointment right before bed because it causes blurred vision.
The most important concept about prescriptions is that they work best when used in combination with a good treatment plan. Many patients turn to prescriptions as a “magic cure,” only to be disappointed. So you want to continue your eyelid hygiene routine and artificial tears, and keep up with the lifestyle changes, even after starting a prescription.
What’s in the Pipeline
There are approximately 10 drugs in the DED pipeline. These new therapeutics focus around the core categories we discussed above. These are reducing inflammation, increasing tear production, stabilizing the tear film, improving corneal nerve function and strengthening the corneal surface. New therapeutics will provide more options for patients.
Putting It All Together
Dry eye disease can impact your life in many ways and treatment can seem daunting without proper supervision and motivation. Patients and eye doctors equally feel frustrated, and turn to prescription drops as a cure-all, often in desperation. However, prescriptions work best when used alongside a good overall treatment plan that includes eyelid hygiene, eye lubrication and lifestyle changes.
What’s Next
We really think everyone should take our Dry Eye 101 course. Find it here!
If you’ve already taken it, amazing! Check out more articles in the Continuing Education section below.