Has an eye doctor (optometrist or ophthalmologist) suggested expressing your meibomian glands to treat clogged or dysfunctional glands? If so, you may be wondering if it is safe and if there are alternatives.
The answer is yes, to both.
While meibomian gland expression is safe, there are alternatives you can try at home. Because symptoms can occur at any time, it’s important to understand all of the available options.
Key Points
- Meibomian glands produce oil to protect and optimize your tear film, which keeps the eyes lubricated and comfortable.
- Disruptions to meibomian glands can lead to discomfort, irritation and eye conditions such as meibomian gland dysfunction and dry eye disease.
- You can help your meibomian glands express naturally with eyelid hygiene techniques, or an eye doctor can manually express meibomian glands with specialized equipment.
Understanding Meibomian Glands
An intricate system of glands in your eyelids is responsible for keeping your eyes lubricated and comfortable through lipid (oil) production.
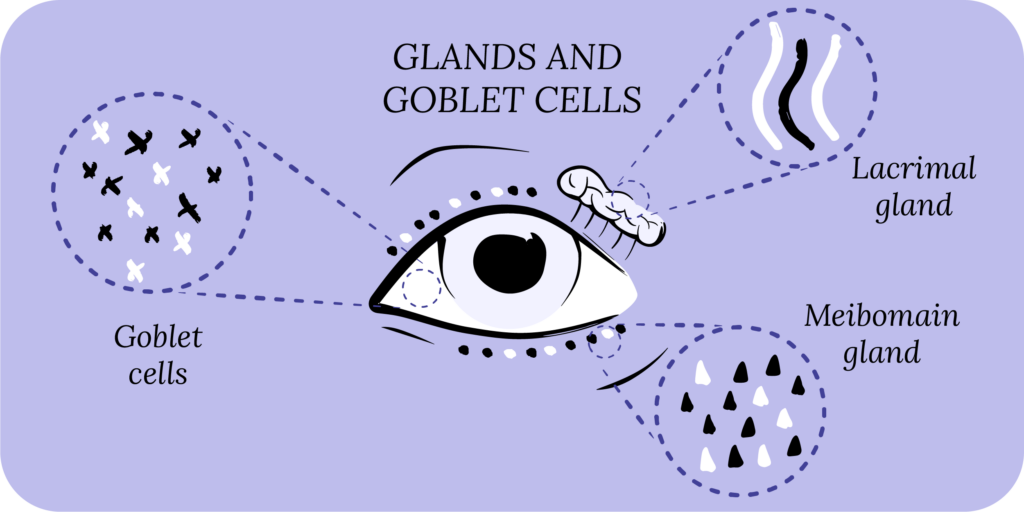
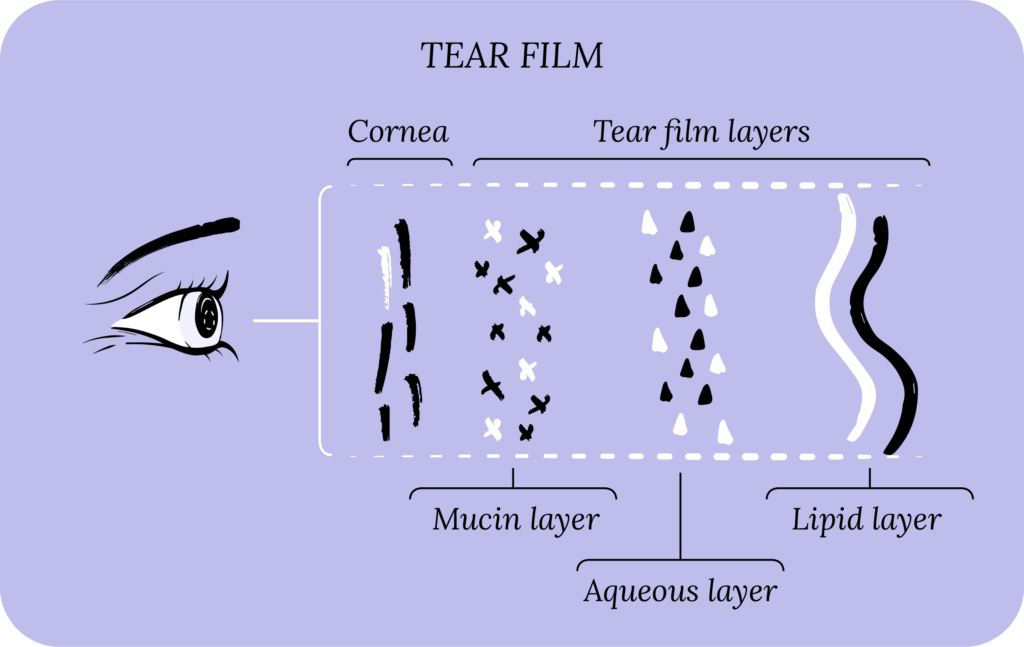
Meibomian glands are oil glands along the edge of the eyelids where they meet the eyelashes.¹ They are located in both the upper lid and lower lid.² These glands secrete oil onto the lid margin called meibum.³ Meibum forms the topmost layer in your tear film, called the lipid layer, and is important for tear stability and in preventing tear evaporation.³
Meibomian glands sometimes stop working well because of various factors. Instead of releasing oil into your tear film, the oil secretions can deposit on the eyelids or in the glands, causing blockages.²
Meibomian Gland Dysfunction (MGD)
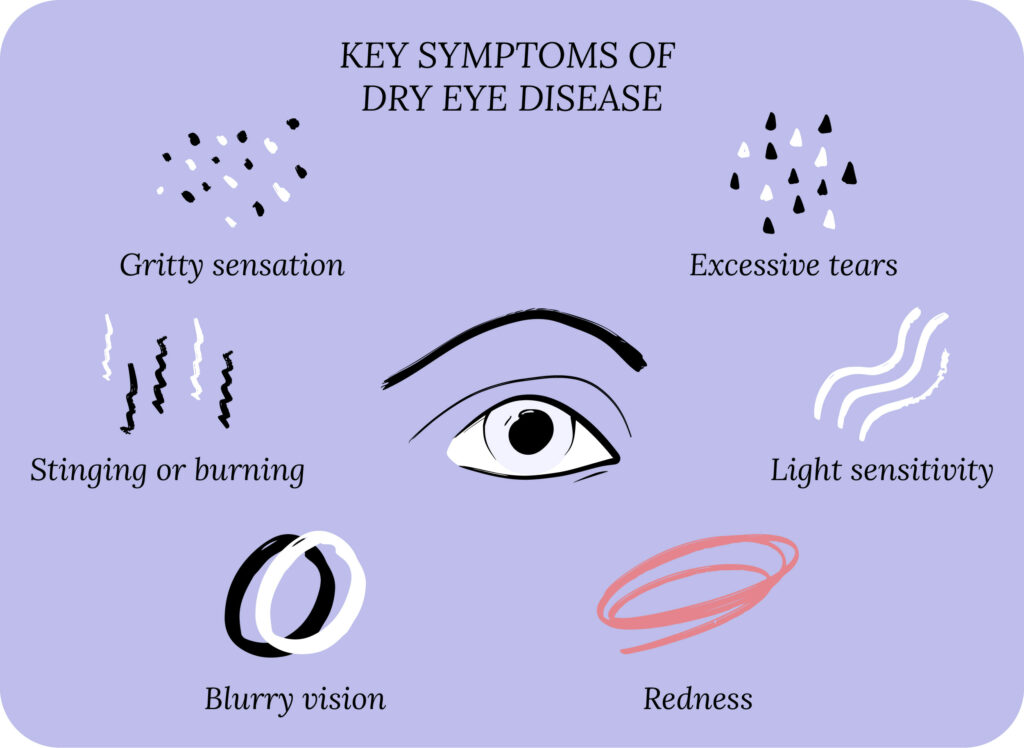
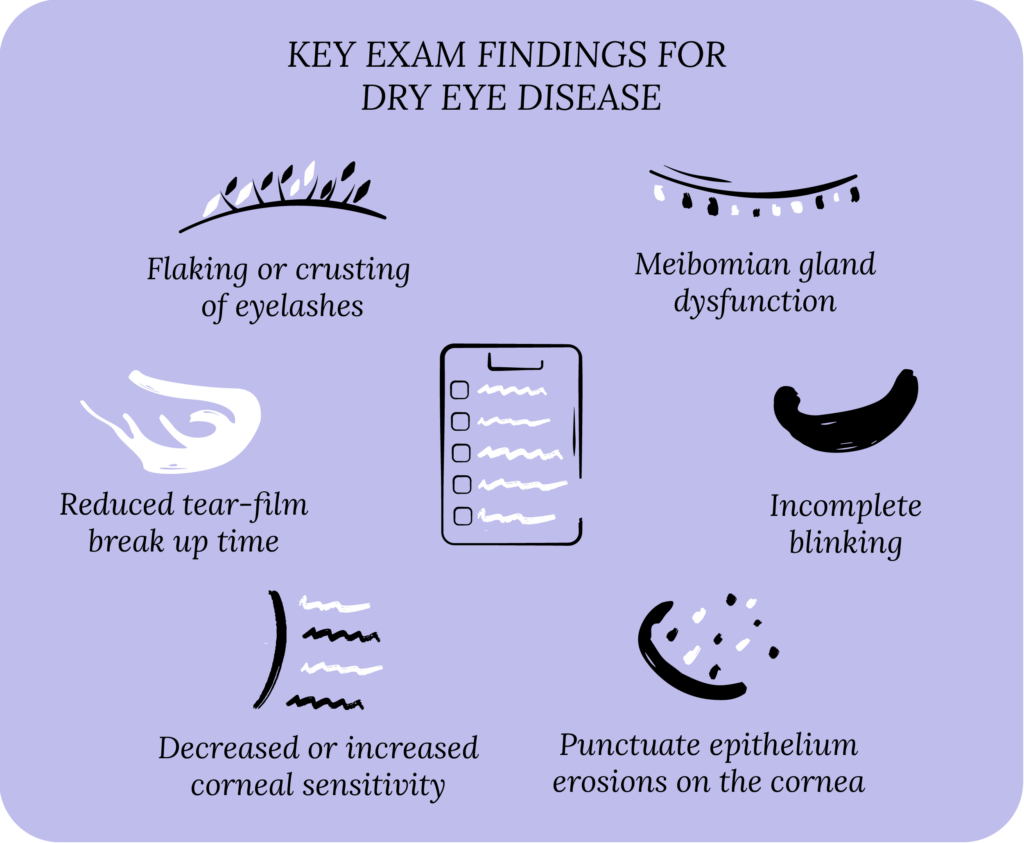
Meibomian Gland Dysfunction (MGD) is a group of related ocular surface disorders. With MGD, oil glands overproduce or underproduce oils needed to lubricate your eyes.² The typical signs of MGD are dry eye symptoms such as dryness, watery eyes, irritation, redness and gritty sensation.⁴
MGD can lead to eyelid inflammation called blepharitis, triggering irritation, burning and redness along the eyelids.⁴ MGD is just one risk factor for blepharitis, more specifically, posterior blepharitis. Rosacea, infections, allergies and dry eyes also contribute to blepharitis.³⁴
Many experts believe MGD is severely underdiagnosed. Age is a contributing factor to MGD and experts predict that over 70% of people over 60 suffer from the disease.²
Causes of MGD
Several conditions and risk factors lead to the development of MGD. Some MGD patients experience symptoms because of multiple factors.
Age
MGD rates increase with age due to meibomian gland atrophy (where meibomian cells die off) as part of the natural aging process. This atrophy leads to disruptions in the cells that produce and release oils.⁴
Environmental and Lifestyle Factors
Living in dry climates with low humidity, smoking cigarettes and having a poor diet lacking omega-3 fatty acids can contribute to MGD.³
Medical Conditions
Autoimmune conditions like Sjögren’s syndrome, which causes severe dry eyes and mouth, can contribute to MGD, as can rosacea and lupus.⁵
Other Eye Conditions
There is overlap between MGD, blepharitis and dry eye disease. It is possible that patients can experience all three at once.⁵
Eye infections, like allergic conjunctivitis (eye allergies), can cause MGD. The meibomian glands become distorted and clogged with oil when the eye is inflamed.⁶
Contact Lens Wear
People who wear contacts are more likely to get MGD. Contact lens wearers have a higher degree of meibomian gland dropout (the loss of meibomian glands), especially with chronic use.³
Treating MGD and Dry Eyes
Treatment for MGD will vary depending on the cause and severity of symptoms. Some people respond well to at-home eye care routines, while others require mechanical/manual expression of meibomian glands.
CorneaCare believes in empowering individuals to take control of their eye health and avoid costly procedures and medications when possible. Eyelid hygiene may be all you need to manage your MGD and dry eyes. However, it can also be an effective tool used in conjunction with medical treatments like in-office meibomian gland expression.
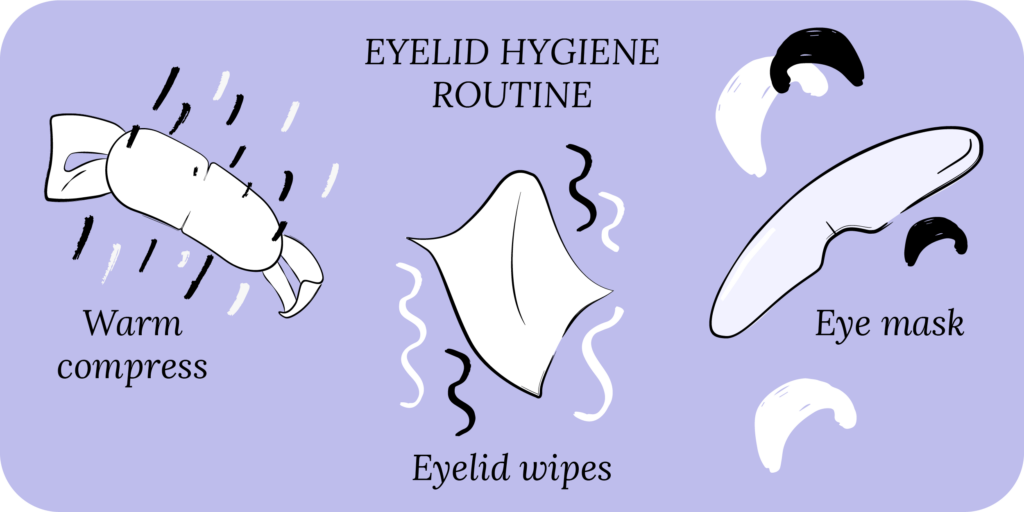
Eyelid Hygiene
More eye doctors now recommend eyelid hygiene as an important tool in treating eye conditions such as dry eye disease, MGD, blepharitis, and eye allergies.
So what is it?
Your eyelids protect your eyes from the outside world. As we’ve learned, they contain glands, oils and tears that help your eyes function and keep them comfortable. Eyelid hygiene is simply caring for your eyelids on a routine (daily) basis much like you do your teeth, skin and hair. It’s important to show them some love!
Even better, eyelid hygiene can improve symptoms associated with MGD, dry eye disease, blepharitis and eye allergies.
5 Simple Eyelid Hygiene Steps to Help with MGD Symptoms
The best part about eyelid hygiene is that you can do it in the privacy and comfort of your home. Trips to the clinic can be inconvenient and expensive. You have tools available to treat your symptoms at home for a fraction of the cost. Here are five eyelid hygiene steps you can start practicing today.
Warm Compress
Warm compresses are a great way to stimulate and open the meibomian glands. They can be made with hot water and a soft washcloth. Simply run the washcloth under hot water, ring out and apply directly to your eyes for 10-15 minutes. You can also make one at home by placing a handful of uncooked rice in a tennis sock, and then heating the tennis sock for about 30-60 seconds.
CorneaCare’s Rest Warm Eye Compresses are self-heating and stay warm longer, so no need to microwave or reheat.

Rest
Warm Compresses
Perfect for eye dryness, fatigue, tearing, and puffiness of the eyelids. Free shipping 📦.
Try today - $30
Cold Compress
Try a cold compress when you have a sudden flare-up of symptoms because cold compresses reduce inflammation and provide immediate relief. Similar to a warm compress, you can make a cold compress at home, except with cold water or an icepack.
Try CorneaCare’s Rescue Hydrogel Self-Cooling Cold Compresses for a convenient, on-the-go cold compress. Made with cooling plant-based extracts, it provides safe and long-lasting relief all without needing a freezer!

Rescue
Cold Compresses
Perfect for sudden flare-ups of eye dryness, pain, burning, and swollen/inflamed eyelids. Free shipping 📦.
Try today - $12
Eyelid Wipes
Because MGD leads to oil secretion disruption, oil often accumulates on the eyelids and leads to blepharitis. Eyelid wipes, like CorneaCare’s Rise Eyelid Wipes, are great for when you first wake up in the morning to help remove build-up from your eyelids. Rise Eyelid Wipes contain natural tea tree oil and hyaluronic acid to combat MGD and blepharitis symptoms naturally.

Rise
Eyelid Wipes
Perfect for eye dryness, itching, burning, and crusting/flaking of eyelashes. Free shipping 📦
Try today - $25
Artificial Tears
If used correctly and consistently, eye drops can be an effective tool in managing MGD symptoms. There are several artificial tears, gels and ointments on the market, so you may have to try a few to experience relief.⁷

Artificial tears can contain preservatives to prolong their shelf-life. The problem is that preservatives can worsen dry eye symptoms if used for a long period. Preservative-free artificial tears are a great alternative but have a shorter shelf life and should be handled with care to avoid spreading bacteria.⁷
Be on the lookout for CorneaCare’s Preservative-free Eye Drops available this summer. With one-way valve technology, germs and bacteria stay outside of the bottle where they belong!
Supplements
Eating a balanced diet rich in healthy fats, fruits, vegetables and whole grains is great for overall health and even better for your eyes! Fatty acids are anti-inflammatory and improve the function of the nerves and nervous tissue in and around your eyes. To ensure you are getting the proper amount of essential fatty acids needed to reduce inflammation, you might try an Omega-3 supplement.
In addition to Omega-3s, adding a multivitamin formulated specifically for the eyes can help reduce symptoms of MGD and dry eyes.
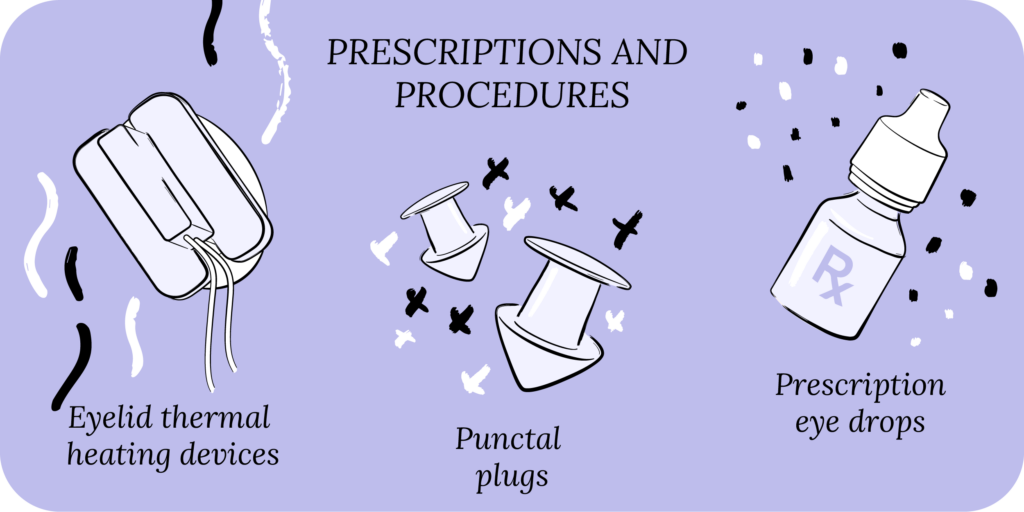
When Meibomian Gland Expression is Necessary
If you’ve tried eyelid hygiene consistently and your symptoms have not improved or have gotten worse, it may be time to discuss meibomian gland expression with your eye doctor. Meibomian gland expression is the act of stimulating the meibomian glands to produce oil or to break up clogged ducts.⁸
Typically, a warm compress (when done consistently) is enough to liquefy the capped oil glands to begin expressing naturally. When that doesn’t work, an eye doctor can manually express meibomian glands in the office by applying gentle force on the eyelids or can use specialized equipment.
How Eye Doctors Express Meibomian Glands
An eye doctor can manually express meibomian glands, or can use heat and light therapy machines.
Your eye doctor will first warm the eyelids using a warm compress or eyelid heating device to loosen the meibum.⁸ They will then apply gentle pressure using a mastrota paddle, cotton swabs or other meibomian gland expressors to the upper and lower eyelids.⁸ Once the doctor has finished the procedure, they will typically apply eye drops and prescribe artificial tear gel to help reduce conjunctiva (outer membrane of the eye) irritation.⁸
Intense Pulsed Light (IPL) therapy is where a machine projects intense, brief bursts of light into the eyelids.⁹ The light causes changes in blood vessels and temperature and can help loosen blockages and stimulate oil production in the meibomian glands.⁹
Lipiflow is a device that is best used for mild to moderate cases of dry eyes, MGD and blepharitis.⁹ The device uses warmth and massage to break up clogged glands and stimulate lipid production.⁹ Its specialized construction protects the cornea from heat and pressure.⁹
Putting It All Together
When it comes to helping your meibomian glands express, you have options. While dry eye symptoms can be frustrating, they shouldn’t interfere with your daily life!
You can manage your symptoms at home and discuss treatments with your eye doctor. Start by practicing one eyelid hygiene step per week, and layer on additional steps until you find your perfect routine.
Make eyecare a part of your self care – your eyes will thank you!
What’s Next
Dry Eye 101 is a comprehensive course designed with you in mind. Begin today to learn how you can take control of your dry eyes for good.